МСКТ или мультиспиральная компьютерная томография — это модификация стандартной компьютерной томографии, которая появилась на свет в 1992 году. В отличие от аналогичной методики, при проведении МСКТ используется модифицированный аппарат, который позволяет быстрее и эффективнее визуализировать ткани.
Мультиспиральная компьютерная томография позволяет визуализировать любые анатомические области с одинаковой эффективностью. Так, МСКТ применяется для диагностики заболеваний сердца, сосудов, внутренних органов. Методика несет минимум опасности, отличается сравнительно малой лучевой нагрузкой организм пациента.
- Показания к проведению МСКТ
- Противопоказания
- Нужна ли специальная подготовка
- Как проводится МСКТ
- Возможные клинические находки
- Отличия МСКТ от стандартной КТ
- Отличия МСКТ от МРТ
- Что же все-таки лучше?
- Недостатки МСКТ
Показания к проведению МСКТ
МСКТ используют для первичной диагностики заболеваний, а также с целью верифицировать ранее установленный диагноз. Подтвердить его с помощью высокоточной методики визуализации.
Мультиспиральная компьютерная томография назначается в нескольких случаях:
- При наличии симптомов, свидетельствующих в пользу органического поражения миокарда. Это может быть кардиомиопатия или перенесенный инфаркт (кардиосклероз). Способ дает много информации о состоянии сердца.
- Если есть проявления, которые могут быть признаками поражения аорты. МСКТ можно назвать золотым стандартом диагностики таких состояний, как расслаивающая аневризма аорты, которая на первых порах протекает с едва заметной симптоматикой. И так пока не станет слишком поздно.
- Признаки поражения почек.
- Симптомы поражения органов брюшной полости.
МСКТ проводится и при предполагаемых поражениях органов мочевыделительного тракта (цистоурография). В основной части случаев методику применяют, когда недостаточно данных для постановки точного диагноза. Или же в тех случаях, когда нужно получить дополнительные данные о состоянии органа, его структуре, анатомических особенностях.
Противопоказания
Противопоказания к МСКТ также имеются:
- Беременность на любом сроке. Поскольку МСКТ при потенциально меньшей лучевой нагрузке все же создает риски для плода. Насколько серьезные — исследователи пока сказать затрудняются.
- Возраст до 14 лет. Поскольку опыт проведения диагностики методом МСКТ при работе с детьми очень скудный. Это лишний риски.
- Психические расстройства, исключающие возможность адекватно мыслить и воспринимать действительность.
- Невозможность сохранять неподвижное положение. При выраженных болях, гиперкинезах или по другим причинам.
- Масса тела более 120 кг. Что связано с техническими характеристиками томографа.
Отдельного разговора заслуживает МСКТ с контрастом. Появляются дополнительные противопоказания: аллергия, выраженная почечная, печеночная, дыхательная недостаточность, проведенное накануне исследования с контрастированием.
Нужна ли специальная подготовка
Специальная подготовка в большинстве случаев не нужна. Достаточно ограничить себя в еде, а за 2–3 часа до исследования, полностью отказаться от пищи.
При обследовании брюшной полости, подготовки стандартная:
- За 3-е суток отказаться от еды, вызывающей повышенное образование кишечного газа. В том числе молока, свежего хлеба и выпечки, многих овощей.
- Накануне сделать микроклизму, а также принять таблетку ветрогонного средства.
Приходить на исследование следует натощак. Желательно взять с собой выписки, заключения, результаты диагностики, чтобы картина врачу была понятна.
Как проводится МСКТ
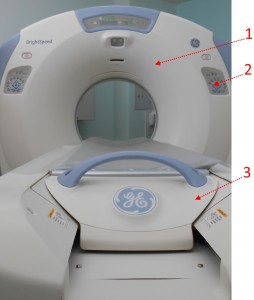
Мультиспиральная томография проводится так же, как и КТ. Пациент ложится на кушетку, его задвигают внутрь аппарата. На протяжении нескольких минут аппарат сканирует организм, после чего строит четкую визуальную картину.
По окончании диагностики пациент остается ждать, получает результаты и может обратиться к своему врачу.
Возможные клинические находки
По результатам диагностики можно обнаружить различные поражения органов и структур. Вот лишь некоторые варианты:
- Рубцовые изменения со стороны сердца. Обычно как следствие перенесенного инфаркта миокарда.
- Кардиомиопатия.
- Пороки сердца, неправильно развитие клапанов.
- Воспалительные поражения сердца.
- Аневризмы аорты.
- Тромбозы аорты.
- Изменения со стороны сосудов сердца. Обнаруживаются при проведении МСКТ-коронарографии.
- Мочекаменная болезнь, структурные аномалии почек.
- Изменения со стороны поджелудочной железы, желчного пузыря и т.д.
- Конкременты в мочевом пузыре, цистит.
МСКТ применяется для детальной визуализации. Методика зарекомендовала себя и в онкологии, как способ диагностики опухолей, раковых процессов и отграничения образований разных типов.
Отличия МСКТ от стандартной КТ
КТ и МСКТ очень похожи в плане методики проведения и диагностической сути. Однако МСКТ появилась позже и заслуженно считается более качественным методом. В отличие от КТ, мультиспиральная компьютерная томография:
- Обладает лучшим качеством картинки. Угол обзора лучше. При желании можно построить подробную трехмерную модель органа пациента. Степень детализации выше, чем у простой компьютерной томографии.
- Требует меньше времени на проведение. Счет идет на минуты. В редких случаях больше.
- Отличается меньшей лучевой нагрузкой. Благодаря усовершенствованному устройству аппарата, пациент меньше времени проводит внутри аппарата. А значит и лучевая нагрузка оказывается ниже.
МСКТ — это идейный продолжатель обычной компьютерной томографии. Способ диагностики нового поколения.
Отличия МСКТ от МРТ
МСКТ и МРТ — принципиально разные исследования. В этом отношении магнитно-резонансная томография отличается и от классической КТ, и от продвинутой МСКТ. Разница представлена в таблице:
|
Мультиспиральная компьютерная томография (МСКТ) |
МРТ |
|
Используется для визуализации костей, твердых минеральных структур. В меньшей мере — мягких тканей. |
Почти не визуализирует костные структуры. Однако отлично показывает состояние мягких тканей. |
|
Эффект базируется на рентгеновском излучении. |
В основе эффекта — ответ атомов водорода при воздействии интенсивного магнитного поля. |
|
Применяется для диагностики заболеваний сосудов, сердца, почек, мочевыделительного тракта. |
Позволяет визуализировать практические любые ткани, кроме костных. Имеет более универсальную и широкую применимость. |
|
Создает вредную лучевую нагрузку |
Не создает никакой лишней нагрузки на организм. |
|
Может проводиться 1–2 раза в год. Плюс-минус по потребности. |
Проводится так часто, как того требует ситуация |
Компьютерная томография имеет те же свойства, что и МСКТ.
Что же все-таки лучше?
Что лучше — зависит от того, какое заболевание предстоит найти. Это вопрос не столько выбора, сколько рациональности, здравого смысла в медицине. Так, бесполезно проводить МРТ при необходимости четко визуализировать кости после перенесенной травмы. Поэтому последнее слово остается за врачом, который видит картину в целом, и знает, что нужно искать.
Недостатки МСКТ
У МСКТ два недостатка, и оба имеют технический характер:
- Во-первых, аппараты для мультиспиральной томографии есть не во всех больницах и даже не во всех регионах.
- Во-вторых, цена на МСКТ выше, чем на КТ.
Что же касается информативности и безопасности, недостатков у МСКТ нет.
This article is about X-ray computed tomography as used in medicine. For cross-sectional images used in industry, see Industrial computed tomography. For means of tomography other than X-ray, see Tomography.
| CT scan | |
|---|---|

Modern CT scanner (2021), photon-counting CT (Siemens NAEOTOM Alpha) |
|
| Other names | X-ray computed tomography (X-ray CT), computerized axial tomography scan (CAT scan),[1] computer aided tomography, computed tomography scan |
| ICD-10-PCS | B?2 |
| ICD-9-CM | 88.38 |
| MeSH | D014057 |
| OPS-301 code | 3–20…3–26 |
| MedlinePlus | 003330 |
|
[edit on Wikidata] |
A computed tomography scan (usually abbreviated to CT scan; formerly called computed axial tomography scan or CAT scan) is a medical imaging technique used to obtain detailed internal images of the body. The personnel that perform CT scans are called radiographers or radiology technologists.[2][3]
CT scanners use a rotating X-ray tube and a row of detectors placed in a gantry to measure X-ray attenuations by different tissues inside the body. The multiple X-ray measurements taken from different angles are then processed on a computer using tomographic reconstruction algorithms to produce tomographic (cross-sectional) images (virtual «slices») of a body. CT scan can be used in patients with metallic implants or pacemakers, for whom magnetic resonance imaging (MRI) is contraindicated.
Since its development in the 1970s, CT scanning has proven to be a versatile imaging technique. While CT is most prominently used in medical diagnosis, it can also be used to form images of non-living objects. The 1979 Nobel Prize in Physiology or Medicine was awarded jointly to South African-American physicist Allan MacLeod Cormack and British electrical engineer Godfrey Hounsfield «for the development of computer-assisted tomography».[4]
Types[edit]
|
|
This section is missing information about dual energy/spectral, fan vs cone beam, dual source ct. Please expand the section to include this information. Further details may exist on the talk page. (November 2021) |
Spiral CT[edit]
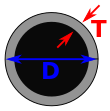
Drawing of CT fan beam and patient in a CT imaging system
CT scan of the thorax. The axial slice (right) is the image that corresponds to number 33 (left).
Spinning tube, commonly called spiral CT, or helical CT, is an imaging technique in which an entire X-ray tube is spun around the central axis of the area being scanned. These are the dominant type of scanners on the market because they have been manufactured longer and offer a lower cost of production and purchase. The main limitation of this type of CT is the bulk and inertia of the equipment (X-ray tube assembly and detector array on the opposite side of the circle) which limits the speed at which the equipment can spin. Some designs use two X-ray sources and detector arrays offset by an angle, as a technique to improve temporal resolution.[5][6]
Electron beam tomography[edit]
Electron beam tomography (EBT) is a specific form of CT in which a large enough X-ray tube is constructed so that only the path of the electrons, travelling between the cathode and anode of the X-ray tube, are spun using deflection coils.[7] This type had a major advantage since sweep speeds can be much faster, allowing for less blurry imaging of moving structures, such as the heart and arteries.[8] Fewer scanners of this design have been produced when compared with spinning tube types, mainly due to the higher cost associated with building a much larger X-ray tube and detector array and limited anatomical coverage.[9]
Dual source CT[edit]
Dual source CT is an advanced scanner with a two X-ray tube detector system, unlike conventional single tube systems.[10][11] These two detector systems are mounted on a single gantry at 90° in the same plane.[12] Dual source Ct scanner allow fast scanning with higher temporal resolution by acquiring a full CT slice in only half a rotation.
Fast imaging reduces motion blurring at high heart rates and potentially allowing for shorter breath-hold time. This is particularly useful for ill patients having difficulty holding their breath or unable to take heart-rate lowering medication.[12][13]
CT perfusion imaging[edit]
CT perfusion imaging is a specific form of CT to assess flow through blood vessels whilst injecting a contrast agent.[14] Blood flow, blood transit time, and organ blood volume, can all be calculated with reasonable sensitivity and specificity.[14] This type of CT may be used on the heart, although sensitivity and specificity for detecting abnormalities are still lower than for other forms of CT.[15] This may also be used on the brain, where CT perfusion imaging can often detect poor brain perfusion well before it is detected using a conventional spiral CT scan.[14][16] This is better for stroke diagnosis than other CT types.[16]
Medical use[edit]
Since its introduction in the 1970s,[17] CT has become an important tool in medical imaging to supplement conventional X-ray imaging and medical ultrasonography. It has more recently been used for preventive medicine or screening for disease, for example, CT colonography for people with a high risk of colon cancer, or full-motion heart scans for people with a high risk of heart disease. Several institutions offer full-body scans for the general population although this practice goes against the advice and official position of many professional organizations in the field primarily due to the radiation dose applied.[18]
The use of CT scans has increased dramatically over the last two decades in many countries.[19] An estimated 72 million scans were performed in the United States in 2007 and more than 80 million in 2015.[20][21]
Head[edit]
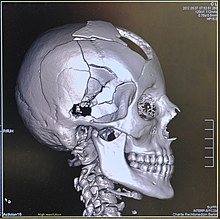
CT scanning of the head is typically used to detect infarction (stroke), tumors, calcifications, haemorrhage, and bone trauma.[22] Of the above, hypodense (dark) structures can indicate edema and infarction, hyperdense (bright) structures indicate calcifications and haemorrhage and bone trauma can be seen as disjunction in bone windows. Tumors can be detected by the swelling and anatomical distortion they cause, or by surrounding edema. CT scanning of the head is also used in CT-guided stereotactic surgery and radiosurgery for treatment of intracranial tumors, arteriovenous malformations, and other surgically treatable conditions using a device known as the N-localizer.[23][24][25][26][27][28]
Neck[edit]
Contrast CT is generally the initial study of choice for neck masses in adults.[29] CT of the thyroid plays an important role in the evaluation of thyroid cancer.[30] CT scan often incidentally finds thyroid abnormalities, and so is often the preferred investigation modality for thyroid abnormalities.[30]
Lungs[edit]
A CT scan can be used for detecting both acute and chronic changes in the lung parenchyma, the tissue of the lungs.[31] It is particularly relevant here because normal two-dimensional X-rays do not show such defects. A variety of techniques are used, depending on the suspected abnormality. For evaluation of chronic interstitial processes such as emphysema, and fibrosis,[32] thin sections with high spatial frequency reconstructions are used; often scans are performed both on inspiration and expiration. This special technique is called high resolution CT that produces a sampling of the lung, and not continuous images.[33]
Bronchial wall thickness (T) and diameter of the bronchus (D)
Bronchial wall thickening can be seen on lung CTs and generally (but not always) implies inflammation of the bronchi.[34]
An incidentally found nodule in the absence of symptoms (sometimes referred to as an incidentaloma) may raise concerns that it might represent a tumor, either benign or malignant.[35] Perhaps persuaded by fear, patients and doctors sometimes agree to an intensive schedule of CT scans, sometimes up to every three months and beyond the recommended guidelines, in an attempt to do surveillance on the nodules.[36] However, established guidelines advise that patients without a prior history of cancer and whose solid nodules have not grown over a two-year period are unlikely to have any malignant cancer.[36] For this reason, and because no research provides supporting evidence that intensive surveillance gives better outcomes, and because of risks associated with having CT scans, patients should not receive CT screening in excess of those recommended by established guidelines.[36]
Angiography[edit]
Example of a CTPA, demonstrating a saddle embolus (dark horizontal line) occluding the pulmonary arteries (bright white triangle)
Computed tomography angiography (CTA) is a type of contrast CT to visualize the arteries and veins throughout the body.[37] This ranges from arteries serving the brain to those bringing blood to the lungs, kidneys, arms and legs. An example of this type of exam is CT pulmonary angiogram (CTPA) used to diagnose pulmonary embolism (PE). It employs computed tomography and an iodine-based contrast agent to obtain an image of the pulmonary arteries.[38][39][40]
Cardiac[edit]
A CT scan of the heart is performed to gain knowledge about cardiac or coronary anatomy.[41] Traditionally, cardiac CT scans are used to detect, diagnose, or follow up coronary artery disease.[42] More recently CT has played a key role in the fast-evolving field of transcatheter structural heart interventions, more specifically in the transcatheter repair and replacement of heart valves.[43][44][45]
The main forms of cardiac CT scanning are:
- Coronary CT angiography (CCTA): the use of CT to assess the coronary arteries of the heart. The subject receives an intravenous injection of radiocontrast, and then the heart is scanned using a high-speed CT scanner, allowing radiologists to assess the extent of occlusion in the coronary arteries, usually to diagnose coronary artery disease.[46][47]
- Coronary CT calcium scan: also used for the assessment of severity of coronary artery disease. Specifically, it looks for calcium deposits in the coronary arteries that can narrow arteries and increase the risk of a heart attack.[48] A typical coronary CT calcium scan is done without the use of radiocontrast, but it can possibly be done from contrast-enhanced images as well.[49]
To better visualize the anatomy, post-processing of the images is common.[42] Most common are multiplanar reconstructions (MPR) and volume rendering. For more complex anatomies and procedures, such as heart valve interventions, a true 3D reconstruction or a 3D print is created based on these CT images to gain a deeper understanding.[50][51][52][53]
Abdomen and pelvis[edit]
CT is an accurate technique for diagnosis of abdominal diseases like Crohn’s disease,[54] GIT bleeding, and diagnosis and staging of cancer, as well as follow-up after cancer treatment to assess response.[55] It is commonly used to investigate acute abdominal pain.[56]
Non-enhanced computed tomography is today the gold standard for diagnosing urinary stones.[57] The size, volume and density of stones can be estimated to help clinicians guide further treatment; size is especially important in predicting spontaneous passage of a stone.[58]
Axial skeleton and extremities[edit]
For the axial skeleton and extremities, CT is often used to image complex fractures, especially ones around joints, because of its ability to reconstruct the area of interest in multiple planes. Fractures, ligamentous injuries, and dislocations can easily be recognized with a 0.2 mm resolution.[59][60] With modern dual-energy CT scanners, new areas of use have been established, such as aiding in the diagnosis of gout.[61]
Biomechanical use[edit]
CT is used in biomechanics to quickly reveal the geometry, anatomy, density and elastic moduli of biological tissues.[62][63]
Other uses[edit]
Industrial use[edit]
Industrial CT scanning (industrial computed tomography) is a process which utilizes X-ray equipment to produce 3D representations of components both externally and internally. Industrial CT scanning has been utilized in many areas of industry for internal inspection of components. Some of the key uses for CT scanning have been flaw detection, failure analysis, metrology, assembly analysis, image-based finite element methods[64] and reverse engineering applications. CT scanning is also employed in the imaging and conservation of museum artifacts.[65]
Aviation security[edit]
CT scanning has also found an application in transport security (predominantly airport security) where it is currently used in a materials analysis context for explosives detection CTX (explosive-detection device)[66][67][68][69] and is also under consideration for automated baggage/parcel security scanning using computer vision based object recognition algorithms that target the detection of specific threat items based on 3D appearance (e.g. guns, knives, liquid containers).[70][71][72] Its usage in airport security pioneered at Shannon Airport in March 2022 has ended the ban on liquids over 100ml there, a move that Heathrow Airport plans for a full roll-out on 1 December 2022 and the TSA spent $781.2 million on an order for over 1,000 scanners, ready to go live in the summer.[73]
Geological use[edit]
X-ray CT is used in geological studies to quickly reveal materials inside a drill core.[74] Dense minerals such as pyrite and barite appear brighter and less dense components such as clay appear dull in CT images.[75]
Cultural heritage use[edit]
X-ray CT and micro-CT can also be used for the conservation and preservation of objects of cultural heritage. For many fragile objects, direct research and observation can be damaging and can degrade the object over time. Using CT scans, conservators and researchers are able to determine the material composition of the objects they are exploring, such as the position of ink along the layers of a scroll, without any additional harm. These scans have been optimal for research focused on the workings of the Antikythera mechanism or the text hidden inside the charred outer layers of the En-Gedi Scroll. However, they are not optimal for every object subject to these kinds of research questions, as there are certain artifacts like the Herculaneum papyri in which the material composition has very little variation along the inside of the object. After scanning these objects, computational methods can be employed to examine the insides of these objects, as was the case with the virtual unwrapping of the En-Gedi scroll and the Herculaneum papyri.[76] Micro-CT has also proved useful for analyzing more recent artifacts such as still-sealed historic correspondence that employed the technique of letterlocking (complex folding and cuts) that provided a «tamper-evident locking mechanism».[77][78] Further examples of use cases in archaeology is imaging the contents of sarcophagi or ceramics.[79]
Micro organism research[edit]
Varied types of fungus can degrade wood to different degrees, one Belgium research group has been used X-ray CT 3 dimension with sub-micron resolution unveiled fungi can penetrate micropores of 0.6 μm[80] under certain conditions.
Interpretation of results[edit]
Presentation[edit]
The result of a CT scan is a volume of voxels, which may be presented to a human observer by various methods, which broadly fit into the following categories:
- Slices (of varying thickness). Thin slice is generally regarded as planes representing a thickness of less than 3 mm.[81][82] Thick slice is generally regarded as planes representing a thickness between 3 mm and 5 mm.[82][83]
- Projection, including maximum intensity projection[84] and average intensity projection
- Volume rendering (VR)[84]
Technically, all volume renderings become projections when viewed on a 2-dimensional display, making the distinction between projections and volume renderings a bit vague. The epitomes of volume rendering models feature a mix of for example coloring and shading in order to create realistic and observable representations.[85][86]
Two-dimensional CT images are conventionally rendered so that the view is as though looking up at it from the patient’s feet.[87] Hence, the left side of the image is to the patient’s right and vice versa, while anterior in the image also is the patient’s anterior and vice versa. This left-right interchange corresponds to the view that physicians generally have in reality when positioned in front of patients.[88]
Grayscale[edit]
Pixels in an image obtained by CT scanning are displayed in terms of relative radiodensity. The pixel itself is displayed according to the mean attenuation of the tissue(s) that it corresponds to on a scale from +3,071 (most attenuating) to −1,024 (least attenuating) on the Hounsfield scale. A pixel is a two dimensional unit based on the matrix size and the field of view. When the CT slice thickness is also factored in, the unit is known as a voxel, which is a three-dimensional unit.[89] Water has an attenuation of 0 Hounsfield units (HU), while air is −1,000 HU, cancellous bone is typically +400 HU, and cranial bone can reach 2,000 HU.[90] The attenuation of metallic implants depends on the atomic number of the element used: Titanium usually has an amount of +1000 HU, iron steel can completely extinguish the X-ray and is, therefore, responsible for well-known line-artifacts in computed tomograms. Artifacts are caused by abrupt transitions between low- and high-density materials, which results in data values that exceed the dynamic range of the processing electronics.[91]
Windowing[edit]
CT data sets have a very high dynamic range which must be reduced for display or printing. This is typically done via a process of «windowing», which maps a range (the «window») of pixel values to a grayscale ramp. For example, CT images of the brain are commonly viewed with a window extending from 0 HU to 80 HU. Pixel values of 0 and lower, are displayed as black; values of 80 and higher are displayed as white; values within the window are displayed as a grey intensity proportional to position within the window.[92] The window used for display must be matched to the X-ray density of the object of interest, in order to optimize the visible detail.[93]
Multiplanar reconstruction and projections[edit]
Typical screen layout for diagnostic software, showing one volume rendering (VR) and multiplanar view of three thin slices in the axial (upper right), sagittal (lower left), and coronal planes (lower right)
Special planes are sometimes useful, such as this oblique longitudinal plane in order to visualize the neuroforamina of the vertebral column, showing narrowing at two levels, causing radiculopathy. The smaller images are axial plane slices.
Multiplanar reconstruction (MPR) is the process of converting data from one anatomical plane (usually transverse) to other planes. It can be used for thin slices as well as projections. Multiplanar reconstruction is possible as present CT scanners provide almost isotropic resolution.[94]
MPR is used almost in every scan. The spine is frequently examined with it.[95] An image of the spine in axial plane can only show one vertebral bone at a time and cannot show its relation with other vertebral bones. By reformatting the data in other planes, visualization of the relative position can be achieved in sagittal and coronal plane.[96]
New software allows the reconstruction of data in non-orthogonal (oblique) planes, which help in the visualization of organs which are not in orthogonal planes.[97][98] It is better suited for visualization of the anatomical structure of the bronchi as they do not lie orthogonal to the direction of the scan.[99]
Curved-plane reconstruction is performed mainly for the evaluation of vessels. This type of reconstruction helps to straighten the bends in a vessel, thereby helping to visualize a whole vessel in a single image or in multiple images. After a vessel has been «straightened», measurements such as cross-sectional area and length can be made. This is helpful in preoperative assessment of a surgical procedure.[100]
For 2D projections used in radiation therapy for quality assurance and planning of external beam radiotherapy, including digitally reconstructed radiographs, see Beam’s eye view.
| Type of projection | Schematic illustration | Examples (10 mm slabs) | Description | Uses |
|---|---|---|---|---|
| Average intensity projection (AIP) | 
|
The average attenuation of each voxel is displayed. The image will get smoother as slice thickness increases. It will look more and more similar to conventional projectional radiography as slice thickness increases. | Useful for identifying the internal structures of a solid organ or the walls of hollow structures, such as intestines. | |
| Maximum intensity projection (MIP) | 
|
The voxel with the highest attenuation is displayed. Therefore, high-attenuating structures such as blood vessels filled with contrast media are enhanced. | Useful for angiographic studies and identification of pulmonary nodules. | |
| Minimum intensity projection (MinIP) | 
|
The voxel with the lowest attenuation is displayed. Therefore, low-attenuating structures such as air spaces are enhanced. | Useful for assessing the lung parenchyma. |
Volume rendering[edit]
3D human skull from computed tomography data
A threshold value of radiodensity is set by the operator (e.g., a level that corresponds to bone). With the help of edge detection image processing algorithms a 3D model can be constructed from the initial data and displayed on screen. Various thresholds can be used to get multiple models, each anatomical component such as muscle, bone and cartilage can be differentiated on the basis of different colours given to them. However, this mode of operation cannot show interior structures.[102]
Surface rendering is limited technique as it displays only the surfaces that meet a particular threshold density, and which are towards the viewer. However, In volume rendering, transparency, colours and shading are used which makes it easy to present a volume in a single image. For example, Pelvic bones could be displayed as semi-transparent, so that, even viewing at an oblique angle one part of the image does not hide another.[103]
Image quality[edit]
Low-dose CT scan of the thorax.
Standard-dose CT scan of the thorax.
Dose versus image quality[edit]
An important issue within radiology today is how to reduce the radiation dose during CT examinations without compromising the image quality. In general, higher radiation doses result in higher-resolution images,[104] while lower doses lead to increased image noise and unsharp images. However, increased dosage raises the adverse side effects, including the risk of radiation-induced cancer – a four-phase abdominal CT gives the same radiation dose as 300 chest X-rays.[105] Several methods that can reduce the exposure to ionizing radiation during a CT scan exist.[106]
- New software technology can significantly reduce the required radiation dose. New iterative tomographic reconstruction algorithms (e.g., iterative Sparse Asymptotic Minimum Variance) could offer super-resolution without requiring higher radiation dose.[107]
- Individualize the examination and adjust the radiation dose to the body type and body organ examined. Different body types and organs require different amounts of radiation.[108]
- Higher resolution is not always suitable, such as detection of small pulmonary masses.[109]
Artifacts[edit]
Although images produced by CT are generally faithful representations of the scanned volume, the technique is susceptible to a number of artifacts, such as the following:[110][111]Chapters 3 and 5
- Streak artifact
- Streaks are often seen around materials that block most X-rays, such as metal or bone. Numerous factors contribute to these streaks: under sampling, photon starvation, motion, beam hardening, and Compton scatter. This type of artifact commonly occurs in the posterior fossa of the brain, or if there are metal implants. The streaks can be reduced using newer reconstruction techniques.[112] Approaches such as metal artifact reduction (MAR) can also reduce this artifact.[113][114] MAR techniques include spectral imaging, where CT images are taken with photons of different energy levels, and then synthesized into monochromatic images with special software such as GSI (Gemstone Spectral Imaging).[115]
- Partial volume effect
- This appears as «blurring» of edges. It is due to the scanner being unable to differentiate between a small amount of high-density material (e.g., bone) and a larger amount of lower density (e.g., cartilage).[116] The reconstruction assumes that the X-ray attenuation within each voxel is homogeneous; this may not be the case at sharp edges. This is most commonly seen in the z-direction (craniocaudal direction), due to the conventional use of highly anisotropic voxels, which have a much lower out-of-plane resolution, than in-plane resolution. This can be partially overcome by scanning using thinner slices, or an isotropic acquisition on a modern scanner.[117]
- Ring artifact
- Probably the most common mechanical artifact, the image of one or many «rings» appears within an image. They are usually caused by the variations in the response from individual elements in a two dimensional X-ray detector due to defect or miscalibration.[118] Ring artifacts can largely be reduced by intensity normalization, also referred to as flat field correction.[119] Remaining rings can be suppressed by a transformation to polar space, where they become linear stripes.[118] A comparative evaluation of ring artefact reduction on X-ray tomography images showed that the method of Sijbers and Postnov can effectively suppress ring artefacts.[120]
- Noise
- This appears as grain on the image and is caused by a low signal to noise ratio. This occurs more commonly when a thin slice thickness is used. It can also occur when the power supplied to the X-ray tube is insufficient to penetrate the anatomy.[121]
- Windmill
- Streaking appearances can occur when the detectors intersect the reconstruction plane. This can be reduced with filters or a reduction in pitch.[122][123]
- Beam hardening
- This can give a «cupped appearance» when grayscale is visualized as height. It occurs because conventional sources, like X-ray tubes emit a polychromatic spectrum. Photons of higher photon energy levels are typically attenuated less. Because of this, the mean energy of the spectrum increases when passing the object, often described as getting «harder». This leads to an effect increasingly underestimating material thickness, if not corrected. Many algorithms exist to correct for this artifact. They can be divided in mono- and multi-material methods.[112][124][125]
Advantages[edit]
CT scanning has several advantages over traditional two-dimensional medical radiography. First, CT eliminates the superimposition of images of structures outside the area of interest.[126] Second, CT scans have greater image resolution, enabling examination of finer details. CT can distinguish between tissues that differ in radiographic density by 1% or less.[127] Third, CT scanning enables multiplanar reformatted imaging: scan data can be visualized in the transverse (or axial), coronal, or sagittal plane, depending on the diagnostic task.[128]
The improved resolution of CT has permitted the development of new investigations. For example, CT angiography avoids the invasive insertion of a catheter. CT scanning can perform a virtual colonoscopy with greater accuracy and less discomfort for the patient than a traditional colonoscopy.[129][130] Virtual colonography is far more accurate than a barium enema for detection of tumors and uses a lower radiation dose.[131]
CT is a moderate- to high-radiation diagnostic technique. The radiation dose for a particular examination depends on multiple factors: volume scanned, patient build, number and type of scan sequences, and desired resolution and image quality.[132] Two helical CT scanning parameters, tube current and pitch, can be adjusted easily and have a profound effect on radiation. CT scanning is more accurate than two-dimensional radiographs in evaluating anterior interbody fusion, although they may still over-read the extent of fusion.[133]
Adverse effects[edit]
Cancer[edit]
The radiation used in CT scans can damage body cells, including DNA molecules, which can lead to radiation-induced cancer.[134] The radiation doses received from CT scans is variable. Compared to the lowest dose x-ray techniques, CT scans can have 100 to 1,000 times higher dose than conventional X-rays.[135] However, a lumbar spine x-ray has a similar dose as a head CT.[136] Articles in the media often exaggerate the relative dose of CT by comparing the lowest-dose x-ray techniques (chest x-ray) with the highest-dose CT techniques. In general, a routine abdominal CT has a radiation dose similar to three years of average background radiation.[137]
Recent[when?] studies on 2.5 million patients[138] and 3.2 million patients[139] have drawn attention to high cumulative doses of more than 100 mSv to patients undergoing recurrent CT scans within a short time span of 1 to 5 years.
Some experts note that CT scans are known to be «overused,» and «there is distressingly little evidence of better health outcomes associated with the current high rate of scans.»[135] On the other hand, a recent paper analyzing the data of patients who received high cumulative doses showed a high degree of appropriate use.[140] This creates an important issue of cancer risk to these patients. Moreover, a highly significant finding that was previously unreported is that some patients received >100 mSv dose from CT scans in a single day,[138] which counteracts existing criticisms some investigators may have on the effects of protracted versus acute exposure.
Early estimates of harm from CT are partly based on similar radiation exposures experienced by those present during the atomic bomb explosions in Japan after the Second World War and those of nuclear industry workers.[134] Some experts project that in the future, between three and five percent of all cancers would result from medical imaging.[135]
An Australian study of 10.9 million people reported that the increased incidence of cancer after CT scan exposure in this cohort was mostly due to irradiation. In this group, one in every 1,800 CT scans was followed by an excess cancer. If the lifetime risk of developing cancer is 40% then the absolute risk rises to 40.05% after a CT.[141][142]
Some studies have shown that publications indicating an increased risk of cancer from typical doses of body CT scans are plagued with serious methodological limitations and several highly improbable results,[143] concluding that no evidence indicates such low doses cause any long-term harm.[144][145][146]
One study estimated that as many as 0.4% of cancers in the United States resulted from CT scans, and that this may have increased to as much as 1.5 to 2% based on the rate of CT use in 2007.[134] Others dispute this estimate,[147] as there is no consensus that the low levels of radiation used in CT scans cause damage. Lower radiation doses are used in many cases, such as in the investigation of renal colic.[148]
A person’s age plays a significant role in the subsequent risk of cancer.[149] Estimated lifetime cancer mortality risks from an abdominal CT of a one-year-old is 0.1%, or 1:1000 scans.[149] The risk for someone who is 40 years old is half that of someone who is 20 years old with substantially less risk in the elderly.[149] The International Commission on Radiological Protection estimates that the risk to a fetus being exposed to 10 mGy (a unit of radiation exposure) increases the rate of cancer before 20 years of age from 0.03% to 0.04% (for reference a CT pulmonary angiogram exposes a fetus to 4 mGy).[150] A 2012 review did not find an association between medical radiation and cancer risk in children noting however the existence of limitations in the evidences over which the review is based.[151]
CT scans can be performed with different settings for lower exposure in children with most manufacturers of CT scans as of 2007 having this function built in.[152] Furthermore, certain conditions can require children to be exposed to multiple CT scans.[134] Current evidence suggests informing parents of the risks of pediatric CT scanning.[153]
Contrast reactions[edit]
In the United States half of CT scans are contrast CTs using intravenously injected radiocontrast agents.[154] The most common reactions from these agents are mild, including nausea, vomiting, and an itching rash. Severe life-threatening reactions may rarely occur.[155] Overall reactions occur in 1 to 3% with nonionic contrast and 4 to 12% of people with ionic contrast.[156] Skin rashes may appear within a week to 3% of people.[155]
The old radiocontrast agents caused anaphylaxis in 1% of cases while the newer, low-osmolar agents cause reactions in 0.01–0.04% of cases.[155][157] Death occurs in about 2 to 30 people per 1,000,000 administrations, with newer agents being safer.[156][158]
There is a higher risk of mortality in those who are female, elderly or in poor health, usually secondary to either anaphylaxis or acute kidney injury.[154]
The contrast agent may induce contrast-induced nephropathy.[159] This occurs in 2 to 7% of people who receive these agents, with greater risk in those who have preexisting kidney failure,[159] preexisting diabetes, or reduced intravascular volume. People with mild kidney impairment are usually advised to ensure full hydration for several hours before and after the injection. For moderate kidney failure, the use of iodinated contrast should be avoided; this may mean using an alternative technique instead of CT. Those with severe kidney failure requiring dialysis require less strict precautions, as their kidneys have so little function remaining that any further damage would not be noticeable and the dialysis will remove the contrast agent; it is normally recommended, however, to arrange dialysis as soon as possible following contrast administration to minimize any adverse effects of the contrast.
In addition to the use of intravenous contrast, orally administered contrast agents are frequently used when examining the abdomen.[160] These are frequently the same as the intravenous contrast agents, merely diluted to approximately 10% of the concentration. However, oral alternatives to iodinated contrast exist, such as very dilute (0.5–1% w/v) barium sulfate suspensions. Dilute barium sulfate has the advantage that it does not cause allergic-type reactions or kidney failure, but cannot be used in patients with suspected bowel perforation or suspected bowel injury, as leakage of barium sulfate from damaged bowel can cause fatal peritonitis.[161]
Side effects from contrast agents, administered intravenously in some CT scans, might impair kidney performance in patients with kidney disease, although this risk is now believed to be lower than previously thought.[162][159]
Scan dose[edit]
| Examination | Typical effective dose (mSv) to the whole body |
Typical absorbed dose (mGy) to the organ in question |
|---|---|---|
| Annual background radiation | 2.4[163] | 2.4[163] |
| Chest X-ray | 0.02[164] | 0.01–0.15[165] |
| Head CT | 1–2[149] | 56[166] |
| Screening mammography | 0.4[150] | 3[134][165] |
| Abdominal CT | 8[164] | 14[166] |
| Chest CT | 5–7[149] | 13[166] |
| CT colonography | 6–11[149] | |
| Chest, abdomen and pelvis CT | 9.9[166] | 12[166] |
| Cardiac CT angiogram | 9–12[149] | 40–100[165] |
| Barium enema | 15[134] | 15[165] |
| Neonatal abdominal CT | 20[134] | 20[165] |
|
Further information: Template:Effective dose by medical imaging type |
The table reports average radiation exposures; however, there can be a wide variation in radiation doses between similar scan types, where the highest dose could be as much as 22 times higher than the lowest dose.[149] A typical plain film X-ray involves radiation dose of 0.01 to 0.15 mGy, while a typical CT can involve 10–20 mGy for specific organs, and can go up to 80 mGy for certain specialized CT scans.[165]
For purposes of comparison, the world average dose rate from naturally occurring sources of background radiation is 2.4 mSv per year, equal for practical purposes in this application to 2.4 mGy per year.[163] While there is some variation, most people (99%) received less than 7 mSv per year as background radiation.[167] Medical imaging as of 2007 accounted for half of the radiation exposure of those in the United States with CT scans making up two thirds of this amount.[149] In the United Kingdom it accounts for 15% of radiation exposure.[150] The average radiation dose from medical sources is ≈0.6 mSv per person globally as of 2007.[149] Those in the nuclear industry in the United States are limited to doses of 50 mSv a year and 100 mSv every 5 years.[149]
Lead is the main material used by radiography personnel for shielding against scattered X-rays.
Radiation dose units[edit]
The radiation dose reported in the gray or mGy unit is proportional to the amount of energy that the irradiated body part is expected to absorb, and the physical effect (such as DNA double strand breaks) on the cells’ chemical bonds by X-ray radiation is proportional to that energy.[168]
The sievert unit is used in the report of the effective dose. The sievert unit, in the context of CT scans, does not correspond to the actual radiation dose that the scanned body part absorbs but to another radiation dose of another scenario, the whole body absorbing the other radiation dose and the other radiation dose being of a magnitude, estimated to have the same probability to induce cancer as the CT scan.[169] Thus, as is shown in the table above, the actual radiation that is absorbed by a scanned body part is often much larger than the effective dose suggests. A specific measure, termed the computed tomography dose index (CTDI), is commonly used as an estimate of the radiation absorbed dose for tissue within the scan region, and is automatically computed by medical CT scanners.[170]
The equivalent dose is the effective dose of a case, in which the whole body would actually absorb the same radiation dose, and the sievert unit is used in its report. In the case of non-uniform radiation, or radiation given to only part of the body, which is common for CT examinations, using the local equivalent dose alone would overstate the biological risks to the entire organism.[171][172][173]
Effects of radiation[edit]
Most adverse health effects of radiation exposure may be grouped in two general categories:
- deterministic effects (harmful tissue reactions) due in large part to the killing/ malfunction of cells following high doses;[174]
- stochastic effects, i.e., cancer and heritable effects involving either cancer development in exposed individuals owing to mutation of somatic cells or heritable disease in their offspring owing to mutation of reproductive (germ) cells.[175]
The added lifetime risk of developing cancer by a single abdominal CT of 8 mSv is estimated to be 0.05%, or 1 one in 2,000.[176]
Because of increased susceptibility of fetuses to radiation exposure, the radiation dosage of a CT scan is an important consideration in the choice of medical imaging in pregnancy.[177][178]
Excess doses[edit]
In October, 2009, the US Food and Drug Administration (FDA) initiated an investigation of brain perfusion CT (PCT) scans, based on radiation burns caused by incorrect settings at one particular facility for this particular type of CT scan. Over 256 patients were exposed to radiations for over 18-month period. Over 40% of them lost patches of hair, and prompted the editorial to call for increased CT quality assurance programs. It was noted that «while unnecessary radiation exposure should be avoided, a medically needed CT scan obtained with appropriate acquisition parameter has benefits that outweigh the radiation risks.»[149][179] Similar problems have been reported at other centers.[149] These incidents are believed to be due to human error.[149]
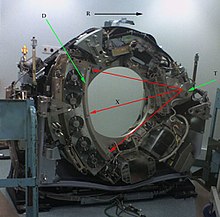
Mechanism[edit]
CT scanner with cover removed to show internal components. Legend:
T: X-ray tube
D: X-ray detectors
X: X-ray beam
R: Gantry rotation
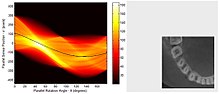
Left image is a sinogram which is a graphic representation of the raw data obtained from a CT scan. At right is an image sample derived from the raw data.[180]
Computed tomography operates by using an X-ray generator that rotates around the object; X-ray detectors are positioned on the opposite side of the circle from the X-ray source.[181] As the X-rays pass through the patient, they are attenuated differently by various tissues according to the tissue density.[182] A visual representation of the raw data obtained is called a sinogram, yet it is not sufficient for interpretation.[183] Once the scan data has been acquired, the data must be processed using a form of tomographic reconstruction, which produces a series of cross-sectional images.[184] These cross-sectional images are made up of small units of pixels or voxels.[185]
Pixels in an image obtained by CT scanning are displayed in terms of relative radiodensity. The pixel itself is displayed according to the mean attenuation of the tissue(s) that it corresponds to on a scale from +3,071 (most attenuating) to −1,024 (least attenuating) on the Hounsfield scale. A pixel is a two dimensional unit based on the matrix size and the field of view. When the CT slice thickness is also factored in, the unit is known as a voxel, which is a three-dimensional unit.[185]
Water has an attenuation of 0 Hounsfield units (HU), while air is −1,000 HU, cancellous bone is typically +400 HU, and cranial bone can reach 2,000 HU or more (os temporale) and can cause artifacts. The attenuation of metallic implants depends on the atomic number of the element used: Titanium usually has an amount of +1000 HU, iron steel can completely extinguish the X-ray and is, therefore, responsible for well-known line-artifacts in computed tomograms. Artifacts are caused by abrupt transitions between low- and high-density materials, which results in data values that exceed the dynamic range of the processing electronics. Two-dimensional CT images are conventionally rendered so that the view is as though looking up at it from the patient’s feet.[87] Hence, the left side of the image is to the patient’s right and vice versa, while anterior in the image also is the patient’s anterior and vice versa. This left-right interchange corresponds to the view that physicians generally have in reality when positioned in front of patients.
Initially, the images generated in CT scans were in the transverse (axial) anatomical plane, perpendicular to the long axis of the body. Modern scanners allow the scan data to be reformatted as images in other planes. Digital geometry processing can generate a three-dimensional image of an object inside the body from a series of two-dimensional radiographic images taken by rotation around a fixed axis.[110] These cross-sectional images are widely used for medical diagnosis and therapy.[186]
Contrast[edit]
Contrast media used for X-ray CT, as well as for plain film X-ray, are called radiocontrasts. Radiocontrasts for CT are, in general, iodine-based.[187] This is useful to highlight structures such as blood vessels that otherwise would be difficult to delineate from their surroundings. Using contrast material can also help to obtain functional information about tissues. Often, images are taken both with and without radiocontrast.[188]
History[edit]
The history of X-ray computed tomography goes back to at least 1917 with the mathematical theory of the Radon transform.[189][190] In October 1963, William H. Oldendorf received a U.S. patent for a «radiant energy apparatus for investigating selected areas of interior objects obscured by dense material».[191] The first commercially viable CT scanner was invented by Godfrey Hounsfield in 1972.[192]
Etymology[edit]
The word «tomography» is derived from the Greek tome (slice) and graphein (to write).[193] Computed tomography was originally known as the «EMI scan» as it was developed in the early 1970s at a research branch of EMI, a company best known today for its music and recording business.[194] It was later known as computed axial tomography (CAT or CT scan) and body section röntgenography.[195]
The term «CAT scan» is no longer used because current CT scans enable for multiplanar reconstructions. This makes «CT scan» the most appropriate term, which is used by radiologists in common vernacular as well as in textbooks and scientific papers.[196][197][198]
In Medical Subject Headings (MeSH), «computed axial tomography» was used from 1977 to 1979, but the current indexing explicitly includes «X-ray» in the title.[199]
The term sinogram was introduced by Paul Edholm and Bertil Jacobson in 1975.[200]
Society and culture[edit]
Campaigns[edit]
In response to increased concern by the public and the ongoing progress of best practices, the Alliance for Radiation Safety in Pediatric Imaging was formed within the Society for Pediatric Radiology. In concert with the American Society of Radiologic Technologists, the American College of Radiology and the American Association of Physicists in Medicine, the Society for Pediatric Radiology developed and launched the Image Gently Campaign which is designed to maintain high-quality imaging studies while using the lowest doses and best radiation safety practices available on pediatric patients.[201] This initiative has been endorsed and applied by a growing list of various professional medical organizations around the world and has received support and assistance from companies that manufacture equipment used in Radiology.
Following upon the success of the Image Gently campaign, the American College of Radiology, the Radiological Society of North America, the American Association of Physicists in Medicine and the American Society of Radiologic Technologists have launched a similar campaign to address this issue in the adult population called Image Wisely.[202]
The World Health Organization and International Atomic Energy Agency (IAEA) of the United Nations have also been working in this area and have ongoing projects designed to broaden best practices and lower patient radiation dose.[203][204]
Prevalence[edit]
Use of CT has increased dramatically over the last two decades.[19] An estimated 72 million scans were performed in the United States in 2007,[20] accounting for close to half of the total per-capita dose rate from radiologic and nuclear medicine procedures.[206] Of the CT scans, six to eleven percent are done in children,[150] an increase of seven to eightfold from 1980.[149] Similar increases have been seen in Europe and Asia.[149] In Calgary, Canada, 12.1% of people who present to the emergency with an urgent complaint received a CT scan, most commonly either of the head or of the abdomen. The percentage who received CT, however, varied markedly by the emergency physician who saw them from 1.8% to 25%.[207] In the emergency department in the United States, CT or MRI imaging is done in 15% of people who present with injuries as of 2007 (up from 6% in 1998).[208]
The increased use of CT scans has been the greatest in two fields: screening of adults (screening CT of the lung in smokers, virtual colonoscopy, CT cardiac screening, and whole-body CT in asymptomatic patients) and CT imaging of children. Shortening of the scanning time to around 1 second, eliminating the strict need for the subject to remain still or be sedated, is one of the main reasons for the large increase in the pediatric population (especially for the diagnosis of appendicitis).[134] As of 2007, in the United States a proportion of CT scans are performed unnecessarily.[152] Some estimates place this number at 30%.[150] There are a number of reasons for this including: legal concerns, financial incentives, and desire by the public.[152] For example, some healthy people avidly pay to receive full-body CT scans as screening. In that case, it is not at all clear that the benefits outweigh the risks and costs. Deciding whether and how to treat incidentalomas is complex, radiation exposure is not negligible, and the money for the scans involves opportunity cost.[152]
Manufacturers[edit]
Major manufacturers of CT Scanners Devices and Equipment are:[209]
Research[edit]
Photon-counting computed tomography is a CT technique currently under development. Typical CT scanners use energy integrating detectors; photons are measured as a voltage on a capacitor which is proportional to the x-rays detected. However, this technique is susceptible to noise and other factors which can affect the linearity of the voltage to x-ray intensity relationship.[210] Photon counting detectors (PCDs) are still affected by noise but it does not change the measured counts of photons. PCDs have several potential advantages, including improving signal (and contrast) to noise ratios, reducing doses, improving spatial resolution, and through use of several energies, distinguishing multiple contrast agents.[211][212] PCDs have only recently become feasible in CT scanners due to improvements in detector technologies that can cope with the volume and rate of data required. As of February 2016, photon counting CT is in use at three sites.[213] Some early research has found the dose reduction potential of photon counting CT for breast imaging to be very promising.[214] In view of recent findings of high cumulative doses to patients from recurrent CT scans, there has been a push for scanning technologies and techniques that reduce ionising radiation doses to patients to sub-milliSievert (sub-mSv in the literature) levels during the CT scan process, a goal that has been lingering.[215][138][139][140]
See also[edit]
- Barium sulfate suspension
- Dosimetry
- Tomosynthesis
- Virtopsy
- X-ray microtomography
- Xenon-enhanced CT scanning
References[edit]
- ^ «CT scan – Mayo Clinic». mayoclinic.org. Archived from the original on 15 October 2016. Retrieved 20 October 2016.
- ^ «Patient Page». ARRT – The American Registry of Radiologic Technologists. Archived from the original on 9 November 2014.
- ^ «Individual State Licensure Information». American Society of Radiologic Technologists. Archived from the original on 18 July 2013. Retrieved 19 July 2013.
- ^ «The Nobel Prize in Physiology or Medicine 1979». NobelPrize.org. Retrieved 2019-08-10.
- ^ Fishman, Elliot K.; Jeffrey, R. Brooke (1995). Spiral CT: Principles, Techniques, and Clinical Applications. Raven Press. ISBN 978-0-7817-0218-8.
- ^ Hsieh, Jiang (2003). Computed Tomography: Principles, Design, Artifacts, and Recent Advances. SPIE Press. p. 265. ISBN 978-0-8194-4425-7.
- ^ Stirrup, James (2020-01-02). Cardiovascular Computed Tomography. Oxford University Press. ISBN 978-0-19-880927-2.
- ^ Talisetti, Anita; Jelnin, Vladimir; Ruiz, Carlos; John, Eunice; Benedetti, Enrico; Testa, Giuliano; Holterman, Ai-Xuan L.; Holterman, Mark J. (December 2004). «Electron beam CT scan is a valuable and safe imaging tool for the pediatric surgical patient». Journal of Pediatric Surgery. 39 (12): 1859–1862. doi:10.1016/j.jpedsurg.2004.08.024. ISSN 1531-5037. PMID 15616951.
- ^ Retsky, Michael (31 July 2008). «Electron beam computed tomography: Challenges and opportunities». Physics Procedia. 1 (1): 149–154. Bibcode:2008PhPro…1..149R. doi:10.1016/j.phpro.2008.07.090.
- ^ Carrascosa, Patricia M.; Cury, Ricardo C.; García, Mario J.; Leipsic, Jonathon A. (2015-10-03). Dual-Energy CT in Cardiovascular Imaging. Springer. ISBN 978-3-319-21227-2.
- ^ Schmidt, Bernhard; Flohr, Thomas (2020-11-01). «Principles and applications of dual source CT». Physica Medica. 125 Years of X-Rays. 79: 36–46. doi:10.1016/j.ejmp.2020.10.014. ISSN 1120-1797. PMID 33115699. S2CID 226056088.
- ^ a b Seidensticker, Peter R.; Hofmann, Lars K. (2008-05-24). Dual Source CT Imaging. Springer Science & Business Media. ISBN 978-3-540-77602-4.
- ^ Schmidt, Bernhard; Flohr, Thomas (2020-11-01). «Principles and applications of dual source CT». Physica Medica: European Journal of Medical Physics. 79: 36–46. doi:10.1016/j.ejmp.2020.10.014. ISSN 1120-1797. PMID 33115699. S2CID 226056088.
- ^ a b c Wittsack, H.-J.; Wohlschläger, A.M.; Ritzl, E.K.; Kleiser, R.; Cohnen, M.; Seitz, R.J.; Mödder, U. (2008-01-01). «CT-perfusion imaging of the human brain: Advanced deconvolution analysis using circulant singular value decomposition». Computerized Medical Imaging and Graphics. 32 (1): 67–77. doi:10.1016/j.compmedimag.2007.09.004. ISSN 0895-6111. PMID 18029143.
- ^ Williams, M.C.; Newby, D.E. (2016-08-01). «CT myocardial perfusion imaging: current status and future directions». Clinical Radiology. 71 (8): 739–749. doi:10.1016/j.crad.2016.03.006. ISSN 0009-9260. PMID 27091433.
- ^ a b Donahue, Joseph; Wintermark, Max (2015-02-01). «Perfusion CT and acute stroke imaging: Foundations, applications, and literature review». Journal of Neuroradiology. 42 (1): 21–29. doi:10.1016/j.neurad.2014.11.003. ISSN 0150-9861. PMID 25636991.
- ^ Curry, Thomas S.; Dowdey, James E.; Murry, Robert C. (1990). Christensen’s Physics of Diagnostic Radiology. Lippincott Williams & Wilkins. p. 289. ISBN 978-0-8121-1310-5.
- ^ «CT Screening» (PDF). hps.org. Archived from the original (PDF) on 13 October 2016. Retrieved 1 May 2018.
- ^ a b Smith-Bindman R, Lipson J, Marcus R, Kim KP, Mahesh M, Gould R, Berrington de González A, Miglioretti DL (December 2009). «Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer». Arch. Intern. Med. 169 (22): 2078–86. doi:10.1001/archinternmed.2009.427. PMC 4635397. PMID 20008690.
- ^ a b Berrington de González A, Mahesh M, Kim KP, Bhargavan M, Lewis R, Mettler F, Land C (December 2009). «Projected cancer risks from computed tomographic scans performed in the United States in 2007». Arch. Intern. Med. 169 (22): 2071–7. doi:10.1001/archinternmed.2009.440. PMC 6276814. PMID 20008689.
- ^ «Dangers of CT Scans and X-Rays – Consumer Reports». Retrieved 16 May 2018.
- ^ Surgeons (AAOS), American Academy of Orthopaedic; Physicians (ACEP), American College of Emergency; UMBC (2017-03-20). Critical Care Transport. Jones & Bartlett Learning. p. 389. ISBN 978-1-284-04099-9.
- ^ Galloway, RL Jr. (2015). «Introduction and Historical Perspectives on Image-Guided Surgery». In Golby, AJ (ed.). Image-Guided Neurosurgery. Amsterdam: Elsevier. pp. 3–4. ISBN 978-0-12-800870-6.
- ^ Tse, VCK; Kalani, MYS; Adler, JR (2015). «Techniques of Stereotactic Localization». In Chin, LS; Regine, WF (eds.). Principles and Practice of Stereotactic Radiosurgery. New York: Springer. p. 28. ISBN 978-0-387-71070-9.
- ^ Saleh, H; Kassas, B (2015). «Developing Stereotactic Frames for Cranial Treatment». In Benedict, SH; Schlesinger, DJ; Goetsch, SJ; Kavanagh, BD (eds.). Stereotactic Radiosurgery and Stereotactic Body Radiation Therapy. Boca Raton: CRC Press. pp. 156–159. ISBN 978-1-4398-4198-3.
- ^ Khan, FR; Henderson, JM (2013). «Deep Brain Stimulation Surgical Techniques». In Lozano, AM; Hallet, M (eds.). Brain Stimulation. Handbook of Clinical Neurology. Vol. 116. Amsterdam: Elsevier. pp. 28–30. doi:10.1016/B978-0-444-53497-2.00003-6. ISBN 978-0-444-53497-2. PMID 24112882.
- ^ Arle, J (2009). «Development of a Classic: the Todd-Wells Apparatus, the BRW, and the CRW Stereotactic Frames». In Lozano, AM; Gildenberg, PL; Tasker, RR (eds.). Textbook of Stereotactic and Functional Neurosurgery. Berlin: Springer-Verlag. pp. 456–461. ISBN 978-3-540-69959-0.
- ^ Brown RA, Nelson JA (June 2012). «Invention of the N-localizer for stereotactic neurosurgery and its use in the Brown-Roberts-Wells stereotactic frame». Neurosurgery. 70 (2 Supplement Operative): 173–176. doi:10.1227/NEU.0b013e318246a4f7. PMID 22186842. S2CID 36350612.
- ^ Daniel G Deschler, Joseph Zenga. «Evaluation of a neck mass in adults». UpToDate. This topic last updated: Dec 04, 2017.
- ^ a b Bin Saeedan, Mnahi; Aljohani, Ibtisam Musallam; Khushaim, Ayman Omar; Bukhari, Salwa Qasim; Elnaas, Salahudin Tayeb (2016). «Thyroid computed tomography imaging: pictorial review of variable pathologies». Insights into Imaging. 7 (4): 601–617. doi:10.1007/s13244-016-0506-5. ISSN 1869-4101. PMC 4956631. PMID 27271508.
- ^ Computed Tomography of the Lung. Springer Berlin Heidelberg. 2007. pp. 40, 47. ISBN 978-3-642-39518-5.
- ^ High-resolution CT of the Lung. Lippincott Williams & Wilkins. 2009. pp. 81, 568. ISBN 978-0-7817-6909-9.
- ^ Martínez-Jiménez, Santiago; Rosado-de-Christenson, Melissa L.; Carter, Brett W. (2017-07-22). Specialty Imaging: HRCT of the Lung E-Book. Elsevier Health Sciences. ISBN 978-0-323-52495-7.
- ^ Yuranga Weerakkody. «Bronchial wall thickening». Radiopaedia. Archived from the original on 2018-01-06. Retrieved 2018-01-05.
- ^ Wiener RS, Gould MK, Woloshin S, Schwartz LM, Clark JA (2012). ««What do you mean, a spot?»: A qualitative analysis of patients’ reactions to discussions with their doctors about pulmonary nodules». Chest. 143 (3): 672–677. doi:10.1378/chest.12-1095. PMC 3590883. PMID 22814873.
- ^ a b c American College of Chest Physicians; American Thoracic Society (September 2013), «Five Things Physicians and Patients Should Question», Choosing Wisely, American College of Chest Physicians and American Thoracic Society, archived from the original on 3 November 2013, retrieved 6 January 2013, which cites
- MacMahon H, Austin JH, Gamsu G, Herold CJ, Jett JR, Naidich DP, Patz EF, Swensen SJ (2005). «Guidelines for Management of Small Pulmonary Nodules Detected on CT Scans: A Statement from the Fleischner Society1». Radiology. 237 (2): 395–400. doi:10.1148/radiol.2372041887. PMID 16244247. S2CID 14498160.
- Gould MK, Fletcher J, Iannettoni MD, Lynch WR, Midthun DE, Naidich DP, Ost DE (2007). «Evaluation of Patients with Pulmonary Nodules: When is It Lung Cancer?*». Chest. 132 (3_suppl): 108S–130S. doi:10.1378/chest.07-1353. PMID 17873164. S2CID 16449420.
- Smith-Bindman R, Lipson J, Marcus R, Kim KP, Mahesh M, Gould R, Berrington de González A, Miglioretti DL (2009). «Radiation Dose Associated with Common Computed Tomography Examinations and the Associated Lifetime Attributable Risk of Cancer». Archives of Internal Medicine. 169 (22): 2078–2086. doi:10.1001/archinternmed.2009.427. PMC 4635397. PMID 20008690.
- Wiener RS, Gould MK, Woloshin S, Schwartz LM, Clark JA (2012). ««What do you mean, a spot?»: A qualitative analysis of patients’ reactions to discussions with their doctors about pulmonary nodules». Chest. 143 (3): 672–677. doi:10.1378/chest.12-1095. PMC 3590883. PMID 22814873.
- ^ McDermott, M.; Jacobs, T.; Morgenstern, L. (2017-01-01), Wijdicks, Eelco F. M.; Kramer, Andreas H. (eds.), «Chapter 10 – Critical care in acute ischemic stroke», Handbook of Clinical Neurology, Critical Care Neurology Part I, Elsevier, 140: 153–176, doi:10.1016/b978-0-444-63600-3.00010-6, PMID 28187798
- ^ «Computed Tomography Angiography (CTA)». www.hopkinsmedicine.org. 19 November 2019. Retrieved 2021-03-21.
- ^ Zeman, R K; Silverman, P M; Vieco, P T; Costello, P (1995-11-01). «CT angiography». American Journal of Roentgenology. 165 (5): 1079–1088. doi:10.2214/ajr.165.5.7572481. ISSN 0361-803X. PMID 7572481.
- ^ Ramalho, Joana; Castillo, Mauricio (2014-03-31). Vascular Imaging of the Central Nervous System: Physical Principles, Clinical Applications, and Emerging Techniques. John Wiley & Sons. p. 69. ISBN 978-1-118-18875-0.
- ^ «Cardiac CT Scan – NHLBI, NIH». www.nhlbi.nih.gov. Archived from the original on 2017-12-01. Retrieved 2017-11-22.
- ^ a b Wichmann, Julian L. «Cardiac CT | Radiology Reference Article | Radiopaedia.org». radiopaedia.org. Archived from the original on 2017-12-01. Retrieved 2017-11-22.
- ^ Marwan, Mohamed; Achenbach, Stephan (February 2016). «Role of Cardiac CT Before Transcatheter Aortic Valve Implantation (TAVI)». Current Cardiology Reports. 18 (2): 21. doi:10.1007/s11886-015-0696-3. ISSN 1534-3170. PMID 26820560. S2CID 41535442.
- ^ Moss, Alastair J.; Dweck, Marc R.; Dreisbach, John G.; Williams, Michelle C.; Mak, Sze Mun; Cartlidge, Timothy; Nicol, Edward D.; Morgan-Hughes, Gareth J. (2016-11-01). «Complementary role of cardiac CT in the assessment of aortic valve replacement dysfunction». Open Heart. 3 (2): e000494. doi:10.1136/openhrt-2016-000494. ISSN 2053-3624. PMC 5093391. PMID 27843568.
- ^ Thériault-Lauzier, Pascal; Spaziano, Marco; Vaquerizo, Beatriz; Buithieu, Jean; Martucci, Giuseppe; Piazza, Nicolo (September 2015). «Computed Tomography for Structural Heart Disease and Interventions». Interventional Cardiology Review. 10 (3): 149–154. doi:10.15420/ICR.2015.10.03.149. ISSN 1756-1477. PMC 5808729. PMID 29588693.
- ^ Passariello, Roberto (2006-03-30). Multidetector-Row CT Angiography. Springer Science & Business Media. ISBN 978-3-540-26984-7.
- ^ Radiology (ACR), Radiological Society of North America (RSNA) and American College of. «Coronary Computed Tomography Angiography (CCTA)». www.radiologyinfo.org. Retrieved 2021-03-19.
- ^ «Heart scan (coronary calcium scan)». Mayo Clinic. Archived from the original on 5 September 2015. Retrieved 9 August 2015.
- ^ van der Bijl, Noortje; Joemai, Raoul M. S.; Geleijns, Jacob; Bax, Jeroen J.; Schuijf, Joanne D.; de Roos, Albert; Kroft, Lucia J. M. (2010). «Assessment of Agatston Coronary Artery Calcium Score Using Contrast-Enhanced CT Coronary Angiography». American Journal of Roentgenology. 195 (6): 1299–1305. doi:10.2214/AJR.09.3734. ISSN 0361-803X. PMID 21098187.
- ^ Vukicevic, Marija; Mosadegh, Bobak; Min, James K.; Little, Stephen H. (February 2017). «Cardiac 3D Printing and its Future Directions». JACC: Cardiovascular Imaging. 10 (2): 171–184. doi:10.1016/j.jcmg.2016.12.001. ISSN 1876-7591. PMC 5664227. PMID 28183437.
- ^ Wang, D. D.; Eng, M.; Greenbaum, A.; Myers, E.; Forbes, M.; Pantelic, M.; Song, T.; Nelson, C.; Divine, G.; Taylor, A.; Wyman, J.; Guerrero, M.; Lederman, R. J.; Paone, G.; O’Neill, W. (2016). «Innovative Mitral Valve Treatment with 3D Visualization at Henry Ford». JACC: Cardiovascular Imaging. 9 (11): 1349–1352. doi:10.1016/j.jcmg.2016.01.017. PMC 5106323. PMID 27209112. Archived from the original on 2017-12-01. Retrieved 2017-11-22.
- ^ Wang, Dee Dee; Eng, Marvin; Greenbaum, Adam; Myers, Eric; Forbes, Michael; Pantelic, Milan; Song, Thomas; Nelson, Christina; Divine, George (November 2016). «Predicting LVOT Obstruction After TMVR». JACC: Cardiovascular Imaging. 9 (11): 1349–1352. doi:10.1016/j.jcmg.2016.01.017. ISSN 1876-7591. PMC 5106323. PMID 27209112.
- ^ Jacobs, Stephan; Grunert, Ronny; Mohr, Friedrich W.; Falk, Volkmar (February 2008). «3D-Imaging of cardiac structures using 3D heart models for planning in heart surgery: a preliminary study». Interactive Cardiovascular and Thoracic Surgery. 7 (1): 6–9. doi:10.1510/icvts.2007.156588. ISSN 1569-9285. PMID 17925319.
- ^ Furukawa, Akira; Saotome, Takao; Yamasaki, Michio; Maeda, Kiyosumi; Nitta, Norihisa; Takahashi, Masashi; Tsujikawa, Tomoyuki; Fujiyama, Yoshihide; Murata, Kiyoshi; Sakamoto, Tsutomu (2004-05-01). «Cross-sectional Imaging in Crohn Disease». RadioGraphics. 24 (3): 689–702. doi:10.1148/rg.243035120. ISSN 0271-5333. PMID 15143222.
- ^ CT of the Acute Abdomen. Springer Berlin Heidelberg. 2011. p. 37. ISBN 978-3-540-89232-8.
- ^ Jay P Heiken; Douglas S Katz (2014). «Emergency Radiology of the Abdomen and Pelvis: Imaging of the Nontraumatic and Traumatic Acute Abdomen». In J. Hodler; R. A. Kubik-Huch; G. K. von Schulthess; Ch. L. Zollikofer (eds.). Diseases of the Abdomen and Pelvis. Springer Milan. p. 3. ISBN 9788847056596.
- ^ Skolarikos, A; Neisius, A; Petřík, A; Somani, B; Thomas, K; Gambaro, G (March 2022). EAU Guidelines on Urolithiasis. Amsterdam: European Association of Urology. ISBN 978-94-92671-16-5.
- ^ Miller, Oren F.; Kane, Christopher J. (September 1999). «Time to stone passage for observed ureteral calculi: a guide for patient education». Journal of Urology. 162 (3 Part 1): 688–691. doi:10.1097/00005392-199909010-00014. PMID 10458343.
- ^ «Ankle Fractures». orthoinfo.aaos.org. American Association of Orthopedic Surgeons. Archived from the original on 30 May 2010. Retrieved 30 May 2010.
- ^ Buckwalter, Kenneth A.; et al. (11 September 2000). «Musculoskeletal Imaging with Multislice CT». American Journal of Roentgenology. 176 (4): 979–986. doi:10.2214/ajr.176.4.1760979. PMID 11264094.
- ^ Ramon, André; Bohm-Sigrand, Amélie; Pottecher, Pierre; Richette, Pascal; Maillefert, Jean-Francis; Devilliers, Herve; Ornetti, Paul (2018-03-01). «Role of dual-energy CT in the diagnosis and follow-up of gout: systematic analysis of the literature». Clinical Rheumatology. 37 (3): 587–595. doi:10.1007/s10067-017-3976-z. ISSN 0770-3198. PMID 29350330. S2CID 3686099.
- ^ Keaveny, Tony M. (March 2010). «Biomechanical computed tomography-noninvasive bone strength analysis using clinical computed tomography scans». Annals of the New York Academy of Sciences. 1192 (1): 57–65. Bibcode:2010NYASA1192…57K. doi:10.1111/j.1749-6632.2009.05348.x. ISSN 1749-6632. PMID 20392218. S2CID 24132358.
- ^ Barber, Asa; Tozzi, Gianluca; Pani, Martino (2019-03-07). Computed Tomography Based Biomechanics. Frontiers Media SA. p. 20. ISBN 978-2-88945-780-9.
- ^ Evans, Ll. M.; Margetts, L.; Casalegno, V.; Lever, L. M.; Bushell, J.; Lowe, T.; Wallwork, A.; Young, P.; Lindemann, A. (2015-05-28). «Transient thermal finite element analysis of CFC–Cu ITER monoblock using X-ray tomography data». Fusion Engineering and Design. 100: 100–111. doi:10.1016/j.fusengdes.2015.04.048. Archived from the original on 2015-10-16.
- ^ Payne, Emma Marie (2012). «Imaging Techniques in Conservation» (PDF). Journal of Conservation and Museum Studies. 10 (2): 17–29. doi:10.5334/jcms.1021201.
- ^ P. Babaheidarian; D. Castanon (2018). «Joint reconstruction and material classification in spectral CT». Anomaly Detection and Imaging with X-Rays (ADIX) III. p. 12. doi:10.1117/12.2309663. ISBN 978-1-5106-1775-9. S2CID 65469251.
- ^ P. Jin; E. Haneda; K. D. Sauer; C. A. Bouman (June 2012). «A model-based 3D multi-slice helical CT reconstruction algorithm for transportation security application» (PDF). Second International Conference on Image Formation in X-Ray Computed Tomography. Archived from the original (PDF) on 2015-04-11. Retrieved 2015-04-05.
- ^ P. Jin; E. Haneda; C. A. Bouman (November 2012). «Implicit Gibbs prior models for tomographic reconstruction» (PDF). Signals, Systems and Computers (ASILOMAR), 2012 Conference Record of the Forty Sixth Asilomar Conference on. IEEE. pp. 613–636. Archived from the original (PDF) on 2015-04-11. Retrieved 2015-04-05.
- ^ S. J. Kisner; P. Jin; C. A. Bouman; K. D. Sauer; W. Garms; T. Gable; S. Oh; M. Merzbacher; S. Skatter (October 2013). «Innovative data weighting for iterative reconstruction in a helical CT security baggage scanner» (PDF). Security Technology (ICCST), 2013 47th International Carnahan Conference on. IEEE. Archived from the original (PDF) on 2015-04-10. Retrieved 2015-04-05.
- ^ Megherbi, N.; Flitton, G.T.; Breckon, T.P. (September 2010). «A Classifier based Approach for the Detection of Potential Threats in CT based Baggage Screening» (PDF). Proc. International Conference on Image Processing. IEEE. pp. 1833–1836. CiteSeerX 10.1.1.188.5206. doi:10.1109/ICIP.2010.5653676. ISBN 978-1-4244-7992-4. S2CID 3679917. Retrieved 5 November 2013.
- ^ Megherbi, N.; Han, J.; Flitton, G.T.; Breckon, T.P. (September 2012). «A Comparison of Classification Approaches for Threat Detection in CT based Baggage Screening» (PDF). Proc. International Conference on Image Processing. IEEE. pp. 3109–3112. CiteSeerX 10.1.1.391.2695. doi:10.1109/ICIP.2012.6467558. ISBN 978-1-4673-2533-2. S2CID 6924816. Retrieved 5 November 2013.
- ^ Flitton, G.T.; Breckon, T.P.; Megherbi, N. (September 2013). «A Comparison of 3D Interest Point Descriptors with Application to Airport Baggage Object Detection in Complex CT Imagery» (PDF). Pattern Recognition. 46 (9): 2420–2436. Bibcode:2013PatRe..46.2420F. doi:10.1016/j.patcog.2013.02.008. hdl:1826/15213. Retrieved 5 November 2013.
- ^ Russell, Molly (30 March 2022). «How Next Generation Airport Scanners Are Ending The 100ml Liquid Rule». Simple Flying. Simple Flying. Retrieved 11 April 2022.
- ^ «Laboratory | About Chikyu | The Deep-sea Scientific Drilling Vessel CHIKYU». www.jamstec.go.jp. Retrieved 2019-10-24.
- ^ Tonai, Satoshi; Kubo, Yusuke; Tsang, Man-Yin; Bowden, Stephen; Ide, Kotaro; Hirose, Takehiro; Kamiya, Nana; Yamamoto, Yuzuru; Yang, Kiho; Yamada, Yasuhiro; Morono, Yuki (2019). «A New Method for Quality Control of Geological Cores by X-Ray Computed Tomography: Application in IODP Expedition 370». Frontiers in Earth Science. 7. doi:10.3389/feart.2019.00117. ISSN 2296-6463. S2CID 171394807.
- ^ Seales, W. B.; Parker, C. S.; Segal, M.; Tov, E.; Shor, P.; Porath, Y. (2016). «From damage to discovery via virtual unwrapping: Reading the scroll from En-Gedi». Science Advances. 2 (9): e1601247. Bibcode:2016SciA….2E1247S. doi:10.1126/sciadv.1601247. ISSN 2375-2548. PMC 5031465. PMID 27679821.
- ^ Castellanos, Sara (2 March 2021). «A Letter Sealed for Centuries Has Been Read—Without Even Opening It». The Wall Street Journal. Retrieved 2 March 2021.
- ^ Dambrogio, Jana; Ghassaei, Amanda; Staraza Smith, Daniel; Jackson, Holly; Demaine, Martin L. (2 March 2021). «Unlocking history through automated virtual unfolding of sealed documents imaged by X-ray microtomography». Nature Communications. 12 (1): 1184. Bibcode:2021NatCo..12.1184D. doi:10.1038/s41467-021-21326-w. PMC 7925573. PMID 33654094.
- ^ Advanced documentation methods in studying Corinthian black-figure vase painting on YouTube showing a Computed Tomography scan and rollout of the aryballos No. G26, archaeological collection, Graz University. The video was rendered using the GigaMesh Software Framework, cf. doi:10.11588/heidok.00025189.
Karl, Stephan; Bayer, Paul; Mara, Hubert; Márton, András (2019), «Advanced Documentation Methods in Studying Corinthian Black-figure Vase Painting» (PDF), Proceedings of the 23rd International Conference on Cultural Heritage and New Technologies (CHNT23), Vienna, Austria, ISBN 978-3-200-06576-5, retrieved 2020-01-09 - ^ Bulcke, Jan Van den; Boone, Matthieu; Acker, Joris Van; Hoorebeke, Luc Van (October 2009). «Three-Dimensional X-Ray Imaging and Analysis of Fungi on and in Wood». Microscopy and Microanalysis. 15 (5): 395–402. Bibcode:2009MiMic..15..395V. doi:10.1017/S1431927609990419. hdl:1854/LU-675607. ISSN 1435-8115. PMID 19709462. S2CID 15637414.
- ^ Goldman, L. W. (2008). «Principles of CT: Multislice CT». Journal of Nuclear Medicine Technology. 36 (2): 57–68. doi:10.2967/jnmt.107.044826. ISSN 0091-4916. PMID 18483143.
- ^ a b Reis, Eduardo Pontes; Nascimento, Felipe; Aranha, Mateus; Mainetti Secol, Fernando; Machado, Birajara; Felix, Marcelo; Stein, Anouk; Amaro, Edson (29 July 2020). «Brain Hemorrhage Extended (BHX): Bounding box extrapolation from thick to thin slice CT images v1.1». PhysioNet. 101 (23): 215–220. doi:10.13026/9cft-hg92.
- ^ Park, S.; Chu, L.C.; Hruban, R.H.; Vogelstein, B.; Kinzler, K.W.; Yuille, A.L.; Fouladi, D.F.; Shayesteh, S.; Ghandili, S.; Wolfgang, C.L.; Burkhart, R.; He, J.; Fishman, E.K.; Kawamoto, S. (2020-09-01). «Differentiating autoimmune pancreatitis from pancreatic ductal adenocarcinoma with CT radiomics features». Diagnostic and Interventional Imaging. 101 (9): 555–564. doi:10.1016/j.diii.2020.03.002. ISSN 2211-5684. PMID 32278586. S2CID 215751181.
- ^ a b Fishman, Elliot K.; Ney, Derek R.; Heath, David G.; Corl, Frank M.; Horton, Karen M.; Johnson, Pamela T. (2006). «Volume Rendering versus Maximum Intensity Projection in CT Angiography: What Works Best, When, and Why». RadioGraphics. 26 (3): 905–922. doi:10.1148/rg.263055186. ISSN 0271-5333. PMID 16702462.
- ^ Silverstein, Jonathan C.; Parsad, Nigel M.; Tsirline, Victor (2008). «Automatic perceptual color map generation for realistic volume visualization». Journal of Biomedical Informatics. 41 (6): 927–935. doi:10.1016/j.jbi.2008.02.008. ISSN 1532-0464. PMC 2651027. PMID 18430609.
- ^ Kobbelt, Leif (2006). Vision, Modeling, and Visualization 2006: Proceedings, November 22-24, 2006, Aachen, Germany. IOS Press. p. 185. ISBN 978-3-89838-081-2.
- ^ a b Computerized Tomography chapter Archived 2016-03-04 at the Wayback Machine at University of Connecticut Health Center.
- ^ Schmidt, Derek; Odland, Rick (September 2004). «Mirror-Image Reversal of Coronal Computed Tomography Scans». The Laryngoscope. 114 (9): 1562–1565. doi:10.1097/00005537-200409000-00011. ISSN 0023-852X. PMID 15475782. S2CID 22320649.
- ^ Brant and Helms’ fundamentals of diagnostic radiology (Fifth ed.). Lippincott Williams & Wilkins. 2018-07-19. p. 1600. ISBN 978-1-4963-6738-9. Retrieved 24 January 2019.
- ^ Arthur W. Toga; John C. Mazziotta, eds. (2002). Brain mapping: the methods (2nd ed.). Amsterdam: Academic Press. ISBN 0-12-693019-8. OCLC 52594824.
- ^ Jerrold T. Bushberg; J. Anthony Seibert; Edwin M. Leidholdt; John M. Boone (2002). The essential physics of medical imaging (2nd ed.). Philadelphia: Lippincott Williams & Wilkins. p. 358. ISBN 0-683-30118-7. OCLC 47177732.
- ^ Kamalian, Shervin; Lev, Michael H.; Gupta, Rajiv (2016-01-01). «Computed tomography imaging and angiography – principles». Handbook of Clinical Neurology. 135: 3–20. doi:10.1016/B978-0-444-53485-9.00001-5. ISBN 978-0-444-53485-9. ISSN 0072-9752. PMID 27432657.
- ^ Stirrup, James (2020-01-02). Cardiovascular Computed Tomography. Oxford University Press. p. 136. ISBN 978-0-19-880927-2.
- ^ Udupa, Jayaram K.; Herman, Gabor T. (1999-09-28). 3D Imaging in Medicine, Second Edition. CRC Press. ISBN 978-0-8493-3179-4.
- ^ Krupski, Witold; Kurys-Denis, Ewa; Matuszewski, Łukasz; Plezia, Bogusław (2007-06-30). «Use of multi-planar reconstruction (MPR) and 3-dimentional [sic] (3D) CT to assess stability criteria in C2 vertebral fractures». Journal of Pre-Clinical and Clinical Research. 1 (1): 80–83. ISSN 1898-2395.
- ^ Tins, Bernhard (2010-10-21). «Technical aspects of CT imaging of the spine». Insights into Imaging. 1 (5–6): 349–359. doi:10.1007/s13244-010-0047-2. ISSN 1869-4101. PMC 3259341. PMID 22347928.
- ^ «CT imaging: Where are we going? (Proceedings)». DVM 360. Retrieved 2021-03-21.
- ^ Wolfson, Nikolaj; Lerner, Alexander; Roshal, Leonid (2016-05-30). Orthopedics in Disasters: Orthopedic Injuries in Natural Disasters and Mass Casualty Events. Springer. ISBN 978-3-662-48950-5.
- ^ Laroia, Archana T; Thompson, Brad H; Laroia, Sandeep T; van Beek, Edwin JR (2010-07-28). «Modern imaging of the tracheo-bronchial tree». World Journal of Radiology. 2 (7): 237–248. doi:10.4329/wjr.v2.i7.237. ISSN 1949-8470. PMC 2998855. PMID 21160663.
- ^ Gong, Jing-Shan; Xu, Jian-Min (2004-07-01). «Role of curved planar reformations using multidetector spiral CT in diagnosis of pancreatic and peripancreatic diseases». World Journal of Gastroenterology. 10 (13): 1943–1947. doi:10.3748/wjg.v10.i13.1943. ISSN 1007-9327. PMC 4572236. PMID 15222042.
- ^ Dalrymple, Neal C.; Prasad, Srinivasa R.; Freckleton, Michael W.; Chintapalli, Kedar N. (September 2005). «Informatics in radiology (infoRAD): introduction to the language of three-dimensional imaging with multidetector CT». Radiographics. 25 (5): 1409–1428. doi:10.1148/rg.255055044. ISSN 1527-1323. PMID 16160120.
- ^ Calhoun, Paul S.; Kuszyk, Brian S.; Heath, David G.; Carley, Jennifer C.; Fishman, Elliot K. (1999-05-01). «Three-dimensional Volume Rendering of Spiral CT Data: Theory and Method». RadioGraphics. 19 (3): 745–764. doi:10.1148/radiographics.19.3.g99ma14745. ISSN 0271-5333. PMID 10336201.
- ^ van Ooijen, P. M. A.; van Geuns, R. J. M.; Rensing, B. J. W. M.; Bongaerts, A. H. H.; de Feyter, P. J.; Oudkerk, M. (January 2003). «Noninvasive Coronary Imaging Using Electron Beam CT: Surface Rendering Versus Volume Rendering». American Journal of Roentgenology. 180 (1): 223–226. doi:10.2214/ajr.180.1.1800223. ISSN 0361-803X. PMID 12490509.
- ^ R. A. Crowther; D. J. DeRosier; A. Klug (1970). «The Reconstruction of a Three-Dimensional Structure from Projections and its Application to Electron Microscopy». Proc. R. Soc. Lond. A. 317 (1530): 319–340. Bibcode:1970RSPSA.317..319C. doi:10.1098/rspa.1970.0119. S2CID 122980366.
- ^ Nickoloff, Edward L.; Alderson, Philip O. (August 2001). «Radiation Exposures to Patients from CT: Reality, Public Perception, and Policy». American Journal of Roentgenology. 177 (2): 285–287. doi:10.2214/ajr.177.2.1770285. ISSN 0361-803X. PMID 11461846.
- ^ Barkan, O; Weill, J; Averbuch, A; Dekel, S. «Adaptive Compressed Tomography Sensing» Archived 2016-03-13 at the Wayback Machine. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition 2013 (pp. 2195–2202).
- ^ Proceedings. IEEE. 1995. p. 10. ISBN 9780780324985.
- ^ «Radiation – Effects on organs of the body (somatic effects)». Encyclopedia Britannica. Retrieved 2021-03-21.
- ^ Simpson G (2009). «Thoracic computed tomography: principles and practice». Australian Prescriber. 32 (4): 4. doi:10.18773/austprescr.2009.049.
- ^ a b Hsieh, Jiang (2003). Computed Tomography: Principles, Design, Artifacts, and Recent Advances. SPIE Press. p. 167. ISBN 978-0-8194-4425-7.
- ^ Bhowmik, Ujjal Kumar; Zafar Iqbal, M.; Adhami, Reza R. (28 May 2012). «Mitigating motion artifacts in FDK based 3D Cone-beam Brain Imaging System using markers». Central European Journal of Engineering. 2 (3): 369–382. Bibcode:2012CEJE….2..369B. doi:10.2478/s13531-012-0011-7.
- ^ a b P. Jin; C. A. Bouman; K. D. Sauer (2013). «A Method for Simultaneous Image Reconstruction and Beam Hardening Correction» (PDF). IEEE Nuclear Science Symp. & Medical Imaging Conf., Seoul, Korea, 2013. Archived from the original (PDF) on 2014-06-06. Retrieved 2014-04-23.
- ^ Boas FE, Fleischmann D (2011). «Evaluation of Two Iterative Techniques for Reducing Metal Artifacts in Computed Tomography». Radiology. 259 (3): 894–902. doi:10.1148/radiol.11101782. PMID 21357521.
- ^ Mouton, A.; Megherbi, N.; Van Slambrouck, K.; Nuyts, J.; Breckon, T.P. (2013). «An Experimental Survey of Metal Artefact Reduction in Computed Tomography» (PDF). Journal of X-Ray Science and Technology. 21 (2): 193–226. doi:10.3233/XST-130372. hdl:1826/8204. PMID 23694911.
- ^ Pessis, Eric; Campagna, Raphaël; Sverzut, Jean-Michel; Bach, Fabienne; Rodallec, Mathieu; Guerini, Henri; Feydy, Antoine; Drapé, Jean-Luc (2013). «Virtual Monochromatic Spectral Imaging with Fast Kilovoltage Switching: Reduction of Metal Artifacts at CT». RadioGraphics. 33 (2): 573–583. doi:10.1148/rg.332125124. ISSN 0271-5333. PMID 23479714.
- ^ González Ballester, Miguel Angel; Zisserman, Andrew P.; Brady, Michael (December 2002). «Estimation of the partial volume effect in MRI». Medical Image Analysis. 6 (4): 389–405. doi:10.1016/s1361-8415(02)00061-0. ISSN 1361-8415. PMID 12494949.
- ^ Goldszal, Alberto F.; Pham, Dzung L. (2000-01-01). «Volumetric Segmentation». Handbook of Medical Imaging: 185–194. doi:10.1016/B978-012077790-7/50016-3. ISBN 978-0-12-077790-7.
- ^ a b Jha, Diwaker (2014). «Adaptive center determination for effective suppression of ring artifacts in tomography images». Applied Physics Letters. 105 (14): 143107. Bibcode:2014ApPhL.105n3107J. doi:10.1063/1.4897441.
- ^ Van Nieuwenhove, V; De Beenhouwer, J; De Carlo, F; Mancini, L; Marone, F; Sijbers, J (2015). «Dynamic intensity normalization using eigen flat fields in X-ray imaging» (PDF). Optics Express. 23 (21): 27975–27989. Bibcode:2015OExpr..2327975V. doi:10.1364/oe.23.027975. hdl:10067/1302930151162165141. PMID 26480456.
- ^ Sijbers J, Postnov A (2004). «Reduction of ring artefacts in high resolution micro-CT reconstructions». Phys Med Biol. 49 (14): N247–53. doi:10.1088/0031-9155/49/14/N06. PMID 15357205. S2CID 12744174.
- ^ Newton, Thomas H.; Potts, D. Gordon (1971). Radiology of the Skull and Brain: Technical aspects of computed tomography. Mosby. pp. 3941–3950. ISBN 978-0-8016-3662-2.
- ^ Brüning, R.; Küttner, A.; Flohr, T. (2006-01-16). Protocols for Multislice CT. Springer Science & Business Media. ISBN 978-3-540-27273-1.
- ^ Peh, Wilfred C. G. (2017-08-11). Pitfalls in Musculoskeletal Radiology. Springer. ISBN 978-3-319-53496-1.
- ^ Van de Casteele E, Van Dyck D, Sijbers J, Raman E (2004). «A model-based correction method for beam hardening artefacts in X-ray microtomography». Journal of X-ray Science and Technology. 12 (1): 43–57. CiteSeerX 10.1.1.460.6487.
- ^ Van Gompel G, Van Slambrouck K, Defrise M, Batenburg KJ, Sijbers J, Nuyts J (2011). «Iterative correction of beam hardening artifacts in CT». Medical Physics. 38 (1): 36–49. Bibcode:2011MedPh..38S..36V. CiteSeerX 10.1.1.464.3547. doi:10.1118/1.3577758. PMID 21978116.
- ^ Mikla, Victor I.; Mikla, Victor V. (2013-08-23). Medical Imaging Technology. Elsevier. p. 37. ISBN 978-0-12-417036-0.
- ^ Radiology for the Dental Professional. Elsevier Mosby. 2008. p. 337. ISBN 978-0-323-03071-7.
- ^ Pasipoularides, Ares (November 2009). Heart’s Vortex: Intracardiac Blood Flow Phenomena. PMPH-USA. p. 595. ISBN 978-1-60795-033-2.
- ^ Heiken, JP; Peterson CM; Menias CO (November 2005). «Virtual colonoscopy for colorectal cancer screening: current status: Wednesday 5 October 2005, 14:00–16:00». Cancer Imaging. International Cancer Imaging Society. 5 (Spec No A): S133–S139. doi:10.1102/1470-7330.2005.0108. PMC 1665314. PMID 16361129.
- ^ Bielen DJ, Bosmans HT, De Wever LL, et al. (September 2005). «Clinical validation of high-resolution fast spin-echo MR colonography after colon distention with air». J Magn Reson Imaging. 22 (3): 400–5. doi:10.1002/jmri.20397. PMID 16106357. S2CID 22167728.
- ^ «CT Colonography». Radiologyinfo.org.
- ^ Žabić S, Wang Q, Morton T, Brown KM (March 2013). «A low dose simulation tool for CT systems with energy integrating detectors». Medical Physics. 40 (3): 031102. Bibcode:2013MedPh..40c1102Z. doi:10.1118/1.4789628. PMID 23464282.
- ^ Brian R. Subach M.D., F.A.C.S et al.»Reliability and accuracy of fine-cut computed tomography scans to determine the status of anterior interbody fusions with metallic cages» Archived 2012-12-08 at the Wayback Machine
- ^ a b c d e f g h Brenner DJ, Hall EJ (November 2007). «Computed tomography – an increasing source of radiation exposure» (PDF). N. Engl. J. Med. 357 (22): 2277–84. doi:10.1056/NEJMra072149. PMID 18046031. S2CID 2760372. Archived (PDF) from the original on 2016-03-04.
- ^ a b c Redberg, Rita F., and Smith-Bindman, Rebecca. «We Are Giving Ourselves Cancer» Archived 2017-07-06 at the Wayback Machine, New York Times, January 30, 2014
- ^ Health, Center for Devices and Radiological. «Medical X-ray Imaging – What are the Radiation Risks from CT?». www.fda.gov. Archived from the original on 5 November 2013. Retrieved 1 May 2018.
- ^ (ACR), Radiological Society of North America (RSNA) and American College of Radiology (February 2021). «Patient Safety – Radiation Dose in X-Ray and CT Exams» (PDF). acr.org. Archived from the original (PDF) on 1 January 2021. Retrieved 6 April 2021.
- ^ a b c Rehani, Madan M.; Yang, Kai; Melick, Emily R.; Heil, John; Šalát, Dušan; Sensakovic, William F.; Liu, Bob (2020). «Patients undergoing recurrent CT scans: assessing the magnitude». European Radiology. 30 (4): 1828–1836. doi:10.1007/s00330-019-06523-y. PMID 31792585. S2CID 208520824.
- ^ a b Brambilla, Marco; Vassileva, Jenia; Kuchcinska, Agnieszka; Rehani, Madan M. (2020). «Multinational data on cumulative radiation exposure of patients from recurrent radiological procedures: call for action». European Radiology. 30 (5): 2493–2501. doi:10.1007/s00330-019-06528-7. PMID 31792583. S2CID 208520544.
- ^ a b Rehani, Madan M.; Melick, Emily R.; Alvi, Raza M.; Doda Khera, Ruhani; Batool-Anwar, Salma; Neilan, Tomas G.; Bettmann, Michael (2020). «Patients undergoing recurrent CT exams: assessment of patients with non-malignant diseases, reasons for imaging and imaging appropriateness». European Radiology. 30 (4): 1839–1846. doi:10.1007/s00330-019-06551-8. PMID 31792584. S2CID 208520463.
- ^ Mathews, J. D.; Forsythe, A. V.; Brady, Z.; Butler, M. W.; Goergen, S. K.; Byrnes, G. B.; Giles, G. G.; Wallace, A. B.; Anderson, P. R.; Guiver, T. A.; McGale, P.; Cain, T. M.; Dowty, J. G.; Bickerstaffe, A. C.; Darby, S. C. (2013). «Cancer risk in 680 000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians». BMJ. 346 (may21 1): f2360. doi:10.1136/bmj.f2360. ISSN 1756-1833. PMC 3660619. PMID 23694687.
- ^ Sasieni, P D; Shelton, J; Ormiston-Smith, N; Thomson, C S; Silcocks, P B (2011). «What is the lifetime risk of developing cancer?: the effect of adjusting for multiple primaries». British Journal of Cancer. 105 (3): 460–465. doi:10.1038/bjc.2011.250. ISSN 0007-0920. PMC 3172907. PMID 21772332.
- ^ Eckel, Laurence J.; Fletcher, Joel G.; Bushberg, Jerrold T.; McCollough, Cynthia H. (2015-10-01). «Answers to Common Questions About the Use and Safety of CT Scans». Mayo Clinic Proceedings. 90 (10): 1380–1392. doi:10.1016/j.mayocp.2015.07.011. ISSN 0025-6196. PMID 26434964.
- ^ «Expert opinion: Are CT scans safe?». ScienceDaily. Retrieved 2019-03-14.
- ^ McCollough, Cynthia H.; Bushberg, Jerrold T.; Fletcher, Joel G.; Eckel, Laurence J. (2015-10-01). «Answers to Common Questions About the Use and Safety of CT Scans». Mayo Clinic Proceedings. 90 (10): 1380–1392. doi:10.1016/j.mayocp.2015.07.011. ISSN 0025-6196. PMID 26434964.
- ^ «No evidence that CT scans, X-rays cause cancer». Medical News Today. 4 February 2016. Retrieved 2019-03-14.
- ^ Kalra, Mannudeep K.; Maher, Michael M.; Rizzo, Stefania; Kanarek, David; Shephard, Jo-Anne O. (April 2004). «Radiation exposure from Chest CT: Issues and Strategies». Journal of Korean Medical Science. 19 (2): 159–166. doi:10.3346/jkms.2004.19.2.159. ISSN 1011-8934. PMC 2822293. PMID 15082885.
- ^ Rob, S.; Bryant, T.; Wilson, I.; Somani, B.K. (2017). «Ultra-low-dose, low-dose, and standard-dose CT of the kidney, ureters, and bladder: is there a difference? Results from a systematic review of the literature». Clinical Radiology. 72 (1): 11–15. doi:10.1016/j.crad.2016.10.005. PMID 27810168.
- ^ a b c d e f g h i j k l m n o p Whaites, Eric (2008-10-10). Radiography and Radiology for Dental Care Professionals E-Book. Elsevier Health Sciences. p. 25. ISBN 978-0-7020-4799-2.
- ^ a b c d e Davies, H. E.; Wathen, C. G.; Gleeson, F. V. (25 February 2011). «The risks of radiation exposure related to diagnostic imaging and how to minimise them». BMJ. 342 (feb25 1): d947. doi:10.1136/bmj.d947. PMID 21355025. S2CID 206894472.
- ^ Baysson H, Etard C, Brisse HJ, Bernier MO (January 2012). «[Diagnostic radiation exposure in children and cancer risk: current knowledge and perspectives]». Archives de Pédiatrie. 19 (1): 64–73. doi:10.1016/j.arcped.2011.10.023. PMID 22130615.
- ^ a b c d Semelka RC, Armao DM, Elias J, Huda W (May 2007). «Imaging strategies to reduce the risk of radiation in CT studies, including selective substitution with MRI». J Magn Reson Imaging. 25 (5): 900–9. doi:10.1002/jmri.20895. PMID 17457809. S2CID 5788891.
- ^ Larson DB, Rader SB, Forman HP, Fenton LZ (August 2007). «Informing parents about CT radiation exposure in children: it’s OK to tell them». Am J Roentgenol. 189 (2): 271–5. doi:10.2214/AJR.07.2248. PMID 17646450. S2CID 25020619.
- ^ a b Namasivayam S, Kalra MK, Torres WE, Small WC (Jul 2006). «Adverse reactions to intravenous iodinated contrast media: a primer for radiologists». Emergency Radiology. 12 (5): 210–5. doi:10.1007/s10140-006-0488-6. PMID 16688432. S2CID 28223134.
- ^ a b c Christiansen C (2005-04-15). «X-ray contrast media – an overview». Toxicology. 209 (2): 185–7. doi:10.1016/j.tox.2004.12.020. PMID 15767033.
- ^ a b Wang H, Wang HS, Liu ZP (October 2011). «Agents that induce pseudo-allergic reaction». Drug Discov Ther. 5 (5): 211–9. doi:10.5582/ddt.2011.v5.5.211. PMID 22466368. S2CID 19001357.
- ^ Drain KL, Volcheck GW (2001). «Preventing and managing drug-induced anaphylaxis». Drug Safety. 24 (11): 843–53. doi:10.2165/00002018-200124110-00005. PMID 11665871. S2CID 24840296.
- ^ Castells, Mariana C., ed. (2010-12-09). Anaphylaxis and hypersensitivity reactions. New York: Humana Press. p. 187. ISBN 978-1-60327-950-5.
- ^ a b c Hasebroock KM, Serkova NJ (April 2009). «Toxicity of MRI and CT contrast agents». Expert Opinion on Drug Metabolism & Toxicology. 5 (4): 403–16. doi:10.1517/17425250902873796. PMID 19368492. S2CID 72557671.
- ^ Rawson, James V.; Pelletier, Allen L. (2013-09-01). «When to Order Contrast-Enhanced CT». American Family Physician. 88 (5): 312–316. ISSN 0002-838X. PMID 24010394.
- ^ Thomsen, Henrik S.; Muller, Robert N.; Mattrey, Robert F. (2012-12-06). Trends in Contrast Media. Springer Science & Business Media. ISBN 978-3-642-59814-2.
- ^ Davenport, Matthew (2020). «Use of Intravenous Iodinated Contrast Media in Patients with Kidney Disease: Consensus Statements from the American College of Radiology and the National Kidney Foundation». Radiology. 294 (3): 660–668. doi:10.1148/radiol.2019192094. PMID 31961246.
- ^ a b c Cuttler JM, Pollycove M (2009). «Nuclear energy and health: and the benefits of low-dose radiation hormesis». Dose-Response. 7 (1): 52–89. doi:10.2203/dose-response.08-024.Cuttler. PMC 2664640. PMID 19343116.
- ^ a b «What are the Radiation Risks from CT?». Food and Drug Administration. 2009. Archived from the original on 2013-11-05.
- ^ a b c d e f Hall EJ, Brenner DJ (May 2008). «Cancer risks from diagnostic radiology». The British Journal of Radiology. 81 (965): 362–78. doi:10.1259/bjr/01948454. PMID 18440940. S2CID 23348032.
- ^ a b c d e Shrimpton, P.C; Miller, H.C; Lewis, M.A; Dunn, M. Doses from Computed Tomography (CT) examinations in the UK – 2003 Review Archived 2011-09-22 at the Wayback Machine
- ^ Michael T. Ryan; Poston, John W., eds. (2005). A half century of health physics. Baltimore, Md.: Lippincott Williams & Wilkins. p. 164. ISBN 978-0-7817-6934-1.
- ^ Polo SE, Jackson SP (March 2011). «Dynamics of DNA damage response proteins at DNA breaks: a focus on protein modifications». Genes Dev. 25 (5): 409–33. doi:10.1101/gad.2021311. PMC 3049283. PMID 21363960.
- ^ The Measurement, Reporting, and Management of Radiation Dose in CT Archived 2017-06-23 at the Wayback Machine «It is a single dose parameter that reflects the risk of a nonuniform exposure in terms of an equivalent whole-body exposure.»
- ^ Hill B, Venning AJ, Baldock C (2005). «A preliminary study of the novel application of normoxic polymer gel dosimeters for the measurement of CTDI on diagnostic X-ray CT scanners». Medical Physics. 32 (6): 1589–1597. Bibcode:2005MedPh..32.1589H. doi:10.1118/1.1925181. PMID 16013718.
- ^ Issa, Ziad F.; Miller, John M.; Zipes, Douglas P. (2019-01-01). «Complications of Catheter Ablation of Cardiac Arrhythmias». Clinical Arrhythmology and Electrophysiology. Elsevier. pp. 1042–1067. doi:10.1016/b978-0-323-52356-1.00032-3. ISBN 978-0-323-52356-1.
- ^ «Absorbed, Equivalent, and Effective Dose – ICRPaedia». icrpaedia.org. Retrieved 2021-03-21.
- ^ Materials, National Research Council (US) Committee on Evaluation of EPA Guidelines for Exposure to Naturally Occurring Radioactive (1999). Radiation Quantities and Units, Definitions, Acronyms. National Academies Press (US).
- ^ Pua, Bradley B.; Covey, Anne M.; Madoff, David C. (2018-12-03). Interventional Radiology: Fundamentals of Clinical Practice. Oxford University Press. ISBN 978-0-19-027624-9.
- ^ Paragraph 55 in: «The 2007 Recommendations of the International Commission on Radiological Protection». International Commission on Radiological Protection. Archived from the original on 2012-11-16. Ann. ICRP 37 (2-4)
- ^ «Do CT scans cause cancer?». Harvard Medical School. March 2013. Archived from the original on 2017-12-09. Retrieved 2017-12-09.
- ^ CDC (2020-06-05). «Radiation and pregnancy: A fact sheet for clinicians». Centers for Disease Control and Prevention. Retrieved 2021-03-21.
- ^ Yoon, Ilsup; Slesinger, Todd L. (2021), «Radiation Exposure In Pregnancy», StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 31869154, retrieved 2021-03-21
- ^ Wintermark M, Lev MH (January 2010). «FDA investigates the safety of brain perfusion CT». AJNR Am J Neuroradiol. 31 (1): 2–3. doi:10.3174/ajnr.A1967. PMC 7964089. PMID 19892810.
- ^ Jun, Kyungtaek; Yoon, Seokhwan (2017). «Alignment Solution for CT Image Reconstruction using Fixed Point and Virtual Rotation Axis». Scientific Reports. 7: 41218. arXiv:1605.04833. Bibcode:2017NatSR…741218J. doi:10.1038/srep41218. ISSN 2045-2322. PMC 5264594. PMID 28120881.
- ^ «Computed Tomography (CT)». www.nibib.nih.gov. Retrieved 2021-03-20.
- ^ Aichinger, Horst; Dierker, Joachim; Joite-Barfuß, Sigrid; Säbel, Manfred (2011-10-25). Radiation Exposure and Image Quality in X-Ray Diagnostic Radiology: Physical Principles and Clinical Applications. Springer Science & Business Media. p. 5. ISBN 978-3-642-11241-6.
- ^ Erdoğan, Hakan (1999). Statistical Image Reconstruction Algorithms Using Paraboloidal Surrogates for PET Transmission Scans. University of Michigan. ISBN 978-0-599-63374-2.
- ^ Themes, U. F. O. (2018-10-07). «CT Image Reconstruction Basics». Radiology Key. Retrieved 2021-03-20.
- ^ a b Stirrup, James (2020-01-02). Cardiovascular Computed Tomography. Oxford University Press. ISBN 978-0-19-880927-2.
- ^ «computed tomography – Definition from the Merriam-Webster Online Dictionary». Archived from the original on 19 September 2011. Retrieved 18 August 2009.
- ^ Webb, W. Richard; Brant, William E.; Major, Nancy M. (2014). Fundamentals of Body CT. Elsevier Health Sciences. p. 152. ISBN 978-0-323-26358-0.
- ^ Webb, Wayne Richard; Brant, William E.; Major, Nancy M. (2006-01-01). Fundamentals of Body CT. Elsevier Health Sciences. p. 168. ISBN 978-1-4160-0030-3.
- ^ Thomas, Adrian M. K.; Banerjee, Arpan K.; Busch, Uwe (2005-12-05). Classic Papers in Modern Diagnostic Radiology. Springer Science & Business Media. ISBN 978-3-540-26988-5.
- ^ Radon J (1 December 1986). «On the determination of functions from their integral values along certain manifolds». IEEE Transactions on Medical Imaging. 5 (4): 170–176. doi:10.1109/TMI.1986.4307775. PMID 18244009. S2CID 26553287.
- ^ Oldendorf WH (1978). «The quest for an image of brain: a brief historical and technical review of brain imaging techniques». Neurology. 28 (6): 517–33. doi:10.1212/wnl.28.6.517. PMID 306588. S2CID 42007208.
- ^ Richmond, Caroline (2004). «Obituary – Sir Godfrey Hounsfield». BMJ. 329 (7467): 687. doi:10.1136/bmj.329.7467.687. PMC 517662.
- ^ Frank Natterer (2001). The Mathematics of Computerized Tomography (Classics in Applied Mathematics). Society for Industrial and Applied Mathematics. p. 8. ISBN 978-0-89871-493-7.
- ^ Sperry, Len (2015-12-14). Mental Health and Mental Disorders: An Encyclopedia of Conditions, Treatments, and Well-Being [3 volumes]: An Encyclopedia of Conditions, Treatments, and Well-Being. ABC-CLIO. p. 259. ISBN 978-1-4408-0383-3.
- ^ Hounsfield, G. N. (1977). «The E.M.I. Scanner». Proceedings of the Royal Society of London. Series B, Biological Sciences. 195 (1119): 281–289. Bibcode:1977RSPSB.195..281H. doi:10.1098/rspb.1977.0008. ISSN 0080-4649. JSTOR 77187. PMID 13396. S2CID 34734270.
- ^ Miñano, Glenn (3 November 2015). «What’s the difference between a CAT-Scan and a CT-Scan? — Cincinnati Children’s Blog». blog.cincinnatichildrens.org. Retrieved 2021-03-19.
- ^ «Difference Between CT Scan and CAT Scan | Difference Between». Retrieved 2021-03-19.
- ^ Conquer Your Headaches. International Headache Management. 1994. p. 115. ISBN 978-0-9636292-5-8.
- ^ «MeSH Browser». meshb.nlm.nih.gov.
- ^ Edholm, Paul; Gabor, Herman (December 1987). «Linograms in Image Reconstruction from Projections». IEEE Transactions on Medical Imaging. MI-6 (4): 301–7. doi:10.1109/tmi.1987.4307847. PMID 18244038. S2CID 20832295.
- ^ «Image Gently». The Alliance for Radiation Safety in Pediatric Imaging. Archived from the original on 9 June 2013. Retrieved 19 July 2013.
- ^ «Image Wisely». Joint Task Force on Adult Radiation Protection. Archived from the original on 21 July 2013. Retrieved 19 July 2013.
- ^ «Optimal levels of radiation for patients». World Health Organization. Archived from the original on 25 May 2013. Retrieved 19 July 2013.
- ^ «Global Initiative on Radiation Safety in Healthcare Settings» (PDF). World Health Organization. Archived (PDF) from the original on 29 October 2013. Retrieved 19 July 2013.
- ^ «Computed tomography (CT) scanners». OECD.
- ^ Fred A. Mettler Jr; Mythreyi Bhargavan; Keith Faulkner; Debbie B. Gilley; Joel E. Gray; Geoffrey S. Ibbott; Jill A. Lipoti; Mahadevappa Mahesh; John L. McCrohan; Michael G. Stabin; Bruce R. Thomadsen; Terry T. Yoshizumi (2009). «Radiologic and Nuclear Medicine Studies in the United States and Worldwide: Frequency, Radiation Dose, and Comparison with Other Radiation Sources — 1950-2007». Radiology. 253 (2): 520–531. doi:10.1148/radiol.2532082010. PMID 19789227.
- ^ Andrew Skelly (Aug 3, 2010). «CT ordering all over the map». The Medical Post.
- ^ Korley FK, Pham JC, Kirsch TD (October 2010). «Use of advanced radiology during visits to US emergency departments for injury-related conditions, 1998–2007». JAMA. 304 (13): 1465–71. doi:10.1001/jama.2010.1408. PMID 20924012.
- ^ «Global Computed Tomography (CT) Scanners Devices and Equipment Market Report 2020: Major Players are GE Healthcare, Koninklijke Philips, Hitachi, Siemens and Canon Medical Systems – ResearchAndMarkets.com». Business Wire. November 7, 2019.
- ^ Jenkins, Ron; Gould, R W; Gedcke, Dale (1995). «Instrumentation». Quantitative x-ray spectrometry (2nd ed.). New York: Dekker. p. 90. ISBN 978-0-8247-9554-2.
- ^ Shikhaliev, Polad M.; Xu, Tong; Molloi, Sabee (2005). «Photon counting computed tomography: Concept and initial results». Medical Physics. 32 (2): 427–36. Bibcode:2005MedPh..32..427S. doi:10.1118/1.1854779. PMID 15789589.
- ^ Taguchi, Katsuyuki; Iwanczyk, Jan S. (2013). «Vision 20/20: Single photon counting x-ray detectors in medical imaging». Medical Physics. 40 (10): 100901. Bibcode:2013MedPh..40j0901T. doi:10.1118/1.4820371. PMC 3786515. PMID 24089889.
- ^ «NIH uses photon-counting CT scanner in patients for the first time». National Institutes of Health. 24 February 2016. Archived from the original on 18 August 2016. Retrieved 28 July 2016.
- ^ «Photon-counting breast CT measures up». medicalphysicsweb. Archived from the original on 2016-07-27. Retrieved 28 July 2016.
- ^ Kachelrieß, Marc; Rehani, Madan M. (March 1, 2020). «Is it possible to kill the radiation risk issue in computed tomography?». Physica Medica: European Journal of Medical Physics. 71: 176–177. doi:10.1016/j.ejmp.2020.02.017. PMID 32163886. S2CID 212692606 – via www.physicamedica.com.
External links[edit]
- Development of CT imaging
- CT Artefacts—PPT by David Platten
- Filler, Aaron (2009-06-30). «The History, Development and Impact of Computed Imaging in Neurological Diagnosis and Neurosurgery: CT, MRI, and DTI». Nature Precedings: 1. doi:10.1038/npre.2009.3267.3. ISSN 1756-0357.
- Boone, John M.; McCollough, Cynthia H. (2021). «Computed tomography turns 50». Physics Today. 74 (9): 34–40. Bibcode:2021PhT….74i..34B. doi:10.1063/PT.3.4834. ISSN 0031-9228. S2CID 239718717.
This article is about X-ray computed tomography as used in medicine. For cross-sectional images used in industry, see Industrial computed tomography. For means of tomography other than X-ray, see Tomography.
| CT scan | |
|---|---|

Modern CT scanner (2021), photon-counting CT (Siemens NAEOTOM Alpha) |
|
| Other names | X-ray computed tomography (X-ray CT), computerized axial tomography scan (CAT scan),[1] computer aided tomography, computed tomography scan |
| ICD-10-PCS | B?2 |
| ICD-9-CM | 88.38 |
| MeSH | D014057 |
| OPS-301 code | 3–20…3–26 |
| MedlinePlus | 003330 |
|
[edit on Wikidata] |
A computed tomography scan (usually abbreviated to CT scan; formerly called computed axial tomography scan or CAT scan) is a medical imaging technique used to obtain detailed internal images of the body. The personnel that perform CT scans are called radiographers or radiology technologists.[2][3]
CT scanners use a rotating X-ray tube and a row of detectors placed in a gantry to measure X-ray attenuations by different tissues inside the body. The multiple X-ray measurements taken from different angles are then processed on a computer using tomographic reconstruction algorithms to produce tomographic (cross-sectional) images (virtual «slices») of a body. CT scan can be used in patients with metallic implants or pacemakers, for whom magnetic resonance imaging (MRI) is contraindicated.
Since its development in the 1970s, CT scanning has proven to be a versatile imaging technique. While CT is most prominently used in medical diagnosis, it can also be used to form images of non-living objects. The 1979 Nobel Prize in Physiology or Medicine was awarded jointly to South African-American physicist Allan MacLeod Cormack and British electrical engineer Godfrey Hounsfield «for the development of computer-assisted tomography».[4]
Types[edit]
|
|
This section is missing information about dual energy/spectral, fan vs cone beam, dual source ct. Please expand the section to include this information. Further details may exist on the talk page. (November 2021) |
Spiral CT[edit]
Drawing of CT fan beam and patient in a CT imaging system
CT scan of the thorax. The axial slice (right) is the image that corresponds to number 33 (left).
Spinning tube, commonly called spiral CT, or helical CT, is an imaging technique in which an entire X-ray tube is spun around the central axis of the area being scanned. These are the dominant type of scanners on the market because they have been manufactured longer and offer a lower cost of production and purchase. The main limitation of this type of CT is the bulk and inertia of the equipment (X-ray tube assembly and detector array on the opposite side of the circle) which limits the speed at which the equipment can spin. Some designs use two X-ray sources and detector arrays offset by an angle, as a technique to improve temporal resolution.[5][6]
Electron beam tomography[edit]
Electron beam tomography (EBT) is a specific form of CT in which a large enough X-ray tube is constructed so that only the path of the electrons, travelling between the cathode and anode of the X-ray tube, are spun using deflection coils.[7] This type had a major advantage since sweep speeds can be much faster, allowing for less blurry imaging of moving structures, such as the heart and arteries.[8] Fewer scanners of this design have been produced when compared with spinning tube types, mainly due to the higher cost associated with building a much larger X-ray tube and detector array and limited anatomical coverage.[9]
Dual source CT[edit]
Dual source CT is an advanced scanner with a two X-ray tube detector system, unlike conventional single tube systems.[10][11] These two detector systems are mounted on a single gantry at 90° in the same plane.[12] Dual source Ct scanner allow fast scanning with higher temporal resolution by acquiring a full CT slice in only half a rotation.
Fast imaging reduces motion blurring at high heart rates and potentially allowing for shorter breath-hold time. This is particularly useful for ill patients having difficulty holding their breath or unable to take heart-rate lowering medication.[12][13]
CT perfusion imaging[edit]
CT perfusion imaging is a specific form of CT to assess flow through blood vessels whilst injecting a contrast agent.[14] Blood flow, blood transit time, and organ blood volume, can all be calculated with reasonable sensitivity and specificity.[14] This type of CT may be used on the heart, although sensitivity and specificity for detecting abnormalities are still lower than for other forms of CT.[15] This may also be used on the brain, where CT perfusion imaging can often detect poor brain perfusion well before it is detected using a conventional spiral CT scan.[14][16] This is better for stroke diagnosis than other CT types.[16]
Medical use[edit]
Since its introduction in the 1970s,[17] CT has become an important tool in medical imaging to supplement conventional X-ray imaging and medical ultrasonography. It has more recently been used for preventive medicine or screening for disease, for example, CT colonography for people with a high risk of colon cancer, or full-motion heart scans for people with a high risk of heart disease. Several institutions offer full-body scans for the general population although this practice goes against the advice and official position of many professional organizations in the field primarily due to the radiation dose applied.[18]
The use of CT scans has increased dramatically over the last two decades in many countries.[19] An estimated 72 million scans were performed in the United States in 2007 and more than 80 million in 2015.[20][21]
Head[edit]
CT scanning of the head is typically used to detect infarction (stroke), tumors, calcifications, haemorrhage, and bone trauma.[22] Of the above, hypodense (dark) structures can indicate edema and infarction, hyperdense (bright) structures indicate calcifications and haemorrhage and bone trauma can be seen as disjunction in bone windows. Tumors can be detected by the swelling and anatomical distortion they cause, or by surrounding edema. CT scanning of the head is also used in CT-guided stereotactic surgery and radiosurgery for treatment of intracranial tumors, arteriovenous malformations, and other surgically treatable conditions using a device known as the N-localizer.[23][24][25][26][27][28]
Neck[edit]
Contrast CT is generally the initial study of choice for neck masses in adults.[29] CT of the thyroid plays an important role in the evaluation of thyroid cancer.[30] CT scan often incidentally finds thyroid abnormalities, and so is often the preferred investigation modality for thyroid abnormalities.[30]
Lungs[edit]
A CT scan can be used for detecting both acute and chronic changes in the lung parenchyma, the tissue of the lungs.[31] It is particularly relevant here because normal two-dimensional X-rays do not show such defects. A variety of techniques are used, depending on the suspected abnormality. For evaluation of chronic interstitial processes such as emphysema, and fibrosis,[32] thin sections with high spatial frequency reconstructions are used; often scans are performed both on inspiration and expiration. This special technique is called high resolution CT that produces a sampling of the lung, and not continuous images.[33]
Bronchial wall thickness (T) and diameter of the bronchus (D)
Bronchial wall thickening can be seen on lung CTs and generally (but not always) implies inflammation of the bronchi.[34]
An incidentally found nodule in the absence of symptoms (sometimes referred to as an incidentaloma) may raise concerns that it might represent a tumor, either benign or malignant.[35] Perhaps persuaded by fear, patients and doctors sometimes agree to an intensive schedule of CT scans, sometimes up to every three months and beyond the recommended guidelines, in an attempt to do surveillance on the nodules.[36] However, established guidelines advise that patients without a prior history of cancer and whose solid nodules have not grown over a two-year period are unlikely to have any malignant cancer.[36] For this reason, and because no research provides supporting evidence that intensive surveillance gives better outcomes, and because of risks associated with having CT scans, patients should not receive CT screening in excess of those recommended by established guidelines.[36]
Angiography[edit]
Example of a CTPA, demonstrating a saddle embolus (dark horizontal line) occluding the pulmonary arteries (bright white triangle)
Computed tomography angiography (CTA) is a type of contrast CT to visualize the arteries and veins throughout the body.[37] This ranges from arteries serving the brain to those bringing blood to the lungs, kidneys, arms and legs. An example of this type of exam is CT pulmonary angiogram (CTPA) used to diagnose pulmonary embolism (PE). It employs computed tomography and an iodine-based contrast agent to obtain an image of the pulmonary arteries.[38][39][40]
Cardiac[edit]
A CT scan of the heart is performed to gain knowledge about cardiac or coronary anatomy.[41] Traditionally, cardiac CT scans are used to detect, diagnose, or follow up coronary artery disease.[42] More recently CT has played a key role in the fast-evolving field of transcatheter structural heart interventions, more specifically in the transcatheter repair and replacement of heart valves.[43][44][45]
The main forms of cardiac CT scanning are:
- Coronary CT angiography (CCTA): the use of CT to assess the coronary arteries of the heart. The subject receives an intravenous injection of radiocontrast, and then the heart is scanned using a high-speed CT scanner, allowing radiologists to assess the extent of occlusion in the coronary arteries, usually to diagnose coronary artery disease.[46][47]
- Coronary CT calcium scan: also used for the assessment of severity of coronary artery disease. Specifically, it looks for calcium deposits in the coronary arteries that can narrow arteries and increase the risk of a heart attack.[48] A typical coronary CT calcium scan is done without the use of radiocontrast, but it can possibly be done from contrast-enhanced images as well.[49]
To better visualize the anatomy, post-processing of the images is common.[42] Most common are multiplanar reconstructions (MPR) and volume rendering. For more complex anatomies and procedures, such as heart valve interventions, a true 3D reconstruction or a 3D print is created based on these CT images to gain a deeper understanding.[50][51][52][53]
Abdomen and pelvis[edit]
CT is an accurate technique for diagnosis of abdominal diseases like Crohn’s disease,[54] GIT bleeding, and diagnosis and staging of cancer, as well as follow-up after cancer treatment to assess response.[55] It is commonly used to investigate acute abdominal pain.[56]
Non-enhanced computed tomography is today the gold standard for diagnosing urinary stones.[57] The size, volume and density of stones can be estimated to help clinicians guide further treatment; size is especially important in predicting spontaneous passage of a stone.[58]
Axial skeleton and extremities[edit]
For the axial skeleton and extremities, CT is often used to image complex fractures, especially ones around joints, because of its ability to reconstruct the area of interest in multiple planes. Fractures, ligamentous injuries, and dislocations can easily be recognized with a 0.2 mm resolution.[59][60] With modern dual-energy CT scanners, new areas of use have been established, such as aiding in the diagnosis of gout.[61]
Biomechanical use[edit]
CT is used in biomechanics to quickly reveal the geometry, anatomy, density and elastic moduli of biological tissues.[62][63]
Other uses[edit]
Industrial use[edit]
Industrial CT scanning (industrial computed tomography) is a process which utilizes X-ray equipment to produce 3D representations of components both externally and internally. Industrial CT scanning has been utilized in many areas of industry for internal inspection of components. Some of the key uses for CT scanning have been flaw detection, failure analysis, metrology, assembly analysis, image-based finite element methods[64] and reverse engineering applications. CT scanning is also employed in the imaging and conservation of museum artifacts.[65]
Aviation security[edit]
CT scanning has also found an application in transport security (predominantly airport security) where it is currently used in a materials analysis context for explosives detection CTX (explosive-detection device)[66][67][68][69] and is also under consideration for automated baggage/parcel security scanning using computer vision based object recognition algorithms that target the detection of specific threat items based on 3D appearance (e.g. guns, knives, liquid containers).[70][71][72] Its usage in airport security pioneered at Shannon Airport in March 2022 has ended the ban on liquids over 100ml there, a move that Heathrow Airport plans for a full roll-out on 1 December 2022 and the TSA spent $781.2 million on an order for over 1,000 scanners, ready to go live in the summer.[73]
Geological use[edit]
X-ray CT is used in geological studies to quickly reveal materials inside a drill core.[74] Dense minerals such as pyrite and barite appear brighter and less dense components such as clay appear dull in CT images.[75]
Cultural heritage use[edit]
X-ray CT and micro-CT can also be used for the conservation and preservation of objects of cultural heritage. For many fragile objects, direct research and observation can be damaging and can degrade the object over time. Using CT scans, conservators and researchers are able to determine the material composition of the objects they are exploring, such as the position of ink along the layers of a scroll, without any additional harm. These scans have been optimal for research focused on the workings of the Antikythera mechanism or the text hidden inside the charred outer layers of the En-Gedi Scroll. However, they are not optimal for every object subject to these kinds of research questions, as there are certain artifacts like the Herculaneum papyri in which the material composition has very little variation along the inside of the object. After scanning these objects, computational methods can be employed to examine the insides of these objects, as was the case with the virtual unwrapping of the En-Gedi scroll and the Herculaneum papyri.[76] Micro-CT has also proved useful for analyzing more recent artifacts such as still-sealed historic correspondence that employed the technique of letterlocking (complex folding and cuts) that provided a «tamper-evident locking mechanism».[77][78] Further examples of use cases in archaeology is imaging the contents of sarcophagi or ceramics.[79]
Micro organism research[edit]
Varied types of fungus can degrade wood to different degrees, one Belgium research group has been used X-ray CT 3 dimension with sub-micron resolution unveiled fungi can penetrate micropores of 0.6 μm[80] under certain conditions.
Interpretation of results[edit]
Presentation[edit]
The result of a CT scan is a volume of voxels, which may be presented to a human observer by various methods, which broadly fit into the following categories:
- Slices (of varying thickness). Thin slice is generally regarded as planes representing a thickness of less than 3 mm.[81][82] Thick slice is generally regarded as planes representing a thickness between 3 mm and 5 mm.[82][83]
- Projection, including maximum intensity projection[84] and average intensity projection
- Volume rendering (VR)[84]
Technically, all volume renderings become projections when viewed on a 2-dimensional display, making the distinction between projections and volume renderings a bit vague. The epitomes of volume rendering models feature a mix of for example coloring and shading in order to create realistic and observable representations.[85][86]
Two-dimensional CT images are conventionally rendered so that the view is as though looking up at it from the patient’s feet.[87] Hence, the left side of the image is to the patient’s right and vice versa, while anterior in the image also is the patient’s anterior and vice versa. This left-right interchange corresponds to the view that physicians generally have in reality when positioned in front of patients.[88]
Grayscale[edit]
Pixels in an image obtained by CT scanning are displayed in terms of relative radiodensity. The pixel itself is displayed according to the mean attenuation of the tissue(s) that it corresponds to on a scale from +3,071 (most attenuating) to −1,024 (least attenuating) on the Hounsfield scale. A pixel is a two dimensional unit based on the matrix size and the field of view. When the CT slice thickness is also factored in, the unit is known as a voxel, which is a three-dimensional unit.[89] Water has an attenuation of 0 Hounsfield units (HU), while air is −1,000 HU, cancellous bone is typically +400 HU, and cranial bone can reach 2,000 HU.[90] The attenuation of metallic implants depends on the atomic number of the element used: Titanium usually has an amount of +1000 HU, iron steel can completely extinguish the X-ray and is, therefore, responsible for well-known line-artifacts in computed tomograms. Artifacts are caused by abrupt transitions between low- and high-density materials, which results in data values that exceed the dynamic range of the processing electronics.[91]
Windowing[edit]
CT data sets have a very high dynamic range which must be reduced for display or printing. This is typically done via a process of «windowing», which maps a range (the «window») of pixel values to a grayscale ramp. For example, CT images of the brain are commonly viewed with a window extending from 0 HU to 80 HU. Pixel values of 0 and lower, are displayed as black; values of 80 and higher are displayed as white; values within the window are displayed as a grey intensity proportional to position within the window.[92] The window used for display must be matched to the X-ray density of the object of interest, in order to optimize the visible detail.[93]
Multiplanar reconstruction and projections[edit]
Typical screen layout for diagnostic software, showing one volume rendering (VR) and multiplanar view of three thin slices in the axial (upper right), sagittal (lower left), and coronal planes (lower right)
Special planes are sometimes useful, such as this oblique longitudinal plane in order to visualize the neuroforamina of the vertebral column, showing narrowing at two levels, causing radiculopathy. The smaller images are axial plane slices.
Multiplanar reconstruction (MPR) is the process of converting data from one anatomical plane (usually transverse) to other planes. It can be used for thin slices as well as projections. Multiplanar reconstruction is possible as present CT scanners provide almost isotropic resolution.[94]
MPR is used almost in every scan. The spine is frequently examined with it.[95] An image of the spine in axial plane can only show one vertebral bone at a time and cannot show its relation with other vertebral bones. By reformatting the data in other planes, visualization of the relative position can be achieved in sagittal and coronal plane.[96]
New software allows the reconstruction of data in non-orthogonal (oblique) planes, which help in the visualization of organs which are not in orthogonal planes.[97][98] It is better suited for visualization of the anatomical structure of the bronchi as they do not lie orthogonal to the direction of the scan.[99]
Curved-plane reconstruction is performed mainly for the evaluation of vessels. This type of reconstruction helps to straighten the bends in a vessel, thereby helping to visualize a whole vessel in a single image or in multiple images. After a vessel has been «straightened», measurements such as cross-sectional area and length can be made. This is helpful in preoperative assessment of a surgical procedure.[100]
For 2D projections used in radiation therapy for quality assurance and planning of external beam radiotherapy, including digitally reconstructed radiographs, see Beam’s eye view.
| Type of projection | Schematic illustration | Examples (10 mm slabs) | Description | Uses |
|---|---|---|---|---|
| Average intensity projection (AIP) | 
|
The average attenuation of each voxel is displayed. The image will get smoother as slice thickness increases. It will look more and more similar to conventional projectional radiography as slice thickness increases. | Useful for identifying the internal structures of a solid organ or the walls of hollow structures, such as intestines. | |
| Maximum intensity projection (MIP) | 
|
The voxel with the highest attenuation is displayed. Therefore, high-attenuating structures such as blood vessels filled with contrast media are enhanced. | Useful for angiographic studies and identification of pulmonary nodules. | |
| Minimum intensity projection (MinIP) | 
|
The voxel with the lowest attenuation is displayed. Therefore, low-attenuating structures such as air spaces are enhanced. | Useful for assessing the lung parenchyma. |
Volume rendering[edit]
3D human skull from computed tomography data
A threshold value of radiodensity is set by the operator (e.g., a level that corresponds to bone). With the help of edge detection image processing algorithms a 3D model can be constructed from the initial data and displayed on screen. Various thresholds can be used to get multiple models, each anatomical component such as muscle, bone and cartilage can be differentiated on the basis of different colours given to them. However, this mode of operation cannot show interior structures.[102]
Surface rendering is limited technique as it displays only the surfaces that meet a particular threshold density, and which are towards the viewer. However, In volume rendering, transparency, colours and shading are used which makes it easy to present a volume in a single image. For example, Pelvic bones could be displayed as semi-transparent, so that, even viewing at an oblique angle one part of the image does not hide another.[103]
Image quality[edit]
Low-dose CT scan of the thorax.
Standard-dose CT scan of the thorax.
Dose versus image quality[edit]
An important issue within radiology today is how to reduce the radiation dose during CT examinations without compromising the image quality. In general, higher radiation doses result in higher-resolution images,[104] while lower doses lead to increased image noise and unsharp images. However, increased dosage raises the adverse side effects, including the risk of radiation-induced cancer – a four-phase abdominal CT gives the same radiation dose as 300 chest X-rays.[105] Several methods that can reduce the exposure to ionizing radiation during a CT scan exist.[106]
- New software technology can significantly reduce the required radiation dose. New iterative tomographic reconstruction algorithms (e.g., iterative Sparse Asymptotic Minimum Variance) could offer super-resolution without requiring higher radiation dose.[107]
- Individualize the examination and adjust the radiation dose to the body type and body organ examined. Different body types and organs require different amounts of radiation.[108]
- Higher resolution is not always suitable, such as detection of small pulmonary masses.[109]
Artifacts[edit]
Although images produced by CT are generally faithful representations of the scanned volume, the technique is susceptible to a number of artifacts, such as the following:[110][111]Chapters 3 and 5
- Streak artifact
- Streaks are often seen around materials that block most X-rays, such as metal or bone. Numerous factors contribute to these streaks: under sampling, photon starvation, motion, beam hardening, and Compton scatter. This type of artifact commonly occurs in the posterior fossa of the brain, or if there are metal implants. The streaks can be reduced using newer reconstruction techniques.[112] Approaches such as metal artifact reduction (MAR) can also reduce this artifact.[113][114] MAR techniques include spectral imaging, where CT images are taken with photons of different energy levels, and then synthesized into monochromatic images with special software such as GSI (Gemstone Spectral Imaging).[115]
- Partial volume effect
- This appears as «blurring» of edges. It is due to the scanner being unable to differentiate between a small amount of high-density material (e.g., bone) and a larger amount of lower density (e.g., cartilage).[116] The reconstruction assumes that the X-ray attenuation within each voxel is homogeneous; this may not be the case at sharp edges. This is most commonly seen in the z-direction (craniocaudal direction), due to the conventional use of highly anisotropic voxels, which have a much lower out-of-plane resolution, than in-plane resolution. This can be partially overcome by scanning using thinner slices, or an isotropic acquisition on a modern scanner.[117]
- Ring artifact
- Probably the most common mechanical artifact, the image of one or many «rings» appears within an image. They are usually caused by the variations in the response from individual elements in a two dimensional X-ray detector due to defect or miscalibration.[118] Ring artifacts can largely be reduced by intensity normalization, also referred to as flat field correction.[119] Remaining rings can be suppressed by a transformation to polar space, where they become linear stripes.[118] A comparative evaluation of ring artefact reduction on X-ray tomography images showed that the method of Sijbers and Postnov can effectively suppress ring artefacts.[120]
- Noise
- This appears as grain on the image and is caused by a low signal to noise ratio. This occurs more commonly when a thin slice thickness is used. It can also occur when the power supplied to the X-ray tube is insufficient to penetrate the anatomy.[121]
- Windmill
- Streaking appearances can occur when the detectors intersect the reconstruction plane. This can be reduced with filters or a reduction in pitch.[122][123]
- Beam hardening
- This can give a «cupped appearance» when grayscale is visualized as height. It occurs because conventional sources, like X-ray tubes emit a polychromatic spectrum. Photons of higher photon energy levels are typically attenuated less. Because of this, the mean energy of the spectrum increases when passing the object, often described as getting «harder». This leads to an effect increasingly underestimating material thickness, if not corrected. Many algorithms exist to correct for this artifact. They can be divided in mono- and multi-material methods.[112][124][125]
Advantages[edit]
CT scanning has several advantages over traditional two-dimensional medical radiography. First, CT eliminates the superimposition of images of structures outside the area of interest.[126] Second, CT scans have greater image resolution, enabling examination of finer details. CT can distinguish between tissues that differ in radiographic density by 1% or less.[127] Third, CT scanning enables multiplanar reformatted imaging: scan data can be visualized in the transverse (or axial), coronal, or sagittal plane, depending on the diagnostic task.[128]
The improved resolution of CT has permitted the development of new investigations. For example, CT angiography avoids the invasive insertion of a catheter. CT scanning can perform a virtual colonoscopy with greater accuracy and less discomfort for the patient than a traditional colonoscopy.[129][130] Virtual colonography is far more accurate than a barium enema for detection of tumors and uses a lower radiation dose.[131]
CT is a moderate- to high-radiation diagnostic technique. The radiation dose for a particular examination depends on multiple factors: volume scanned, patient build, number and type of scan sequences, and desired resolution and image quality.[132] Two helical CT scanning parameters, tube current and pitch, can be adjusted easily and have a profound effect on radiation. CT scanning is more accurate than two-dimensional radiographs in evaluating anterior interbody fusion, although they may still over-read the extent of fusion.[133]
Adverse effects[edit]
Cancer[edit]
The radiation used in CT scans can damage body cells, including DNA molecules, which can lead to radiation-induced cancer.[134] The radiation doses received from CT scans is variable. Compared to the lowest dose x-ray techniques, CT scans can have 100 to 1,000 times higher dose than conventional X-rays.[135] However, a lumbar spine x-ray has a similar dose as a head CT.[136] Articles in the media often exaggerate the relative dose of CT by comparing the lowest-dose x-ray techniques (chest x-ray) with the highest-dose CT techniques. In general, a routine abdominal CT has a radiation dose similar to three years of average background radiation.[137]
Recent[when?] studies on 2.5 million patients[138] and 3.2 million patients[139] have drawn attention to high cumulative doses of more than 100 mSv to patients undergoing recurrent CT scans within a short time span of 1 to 5 years.
Some experts note that CT scans are known to be «overused,» and «there is distressingly little evidence of better health outcomes associated with the current high rate of scans.»[135] On the other hand, a recent paper analyzing the data of patients who received high cumulative doses showed a high degree of appropriate use.[140] This creates an important issue of cancer risk to these patients. Moreover, a highly significant finding that was previously unreported is that some patients received >100 mSv dose from CT scans in a single day,[138] which counteracts existing criticisms some investigators may have on the effects of protracted versus acute exposure.
Early estimates of harm from CT are partly based on similar radiation exposures experienced by those present during the atomic bomb explosions in Japan after the Second World War and those of nuclear industry workers.[134] Some experts project that in the future, between three and five percent of all cancers would result from medical imaging.[135]
An Australian study of 10.9 million people reported that the increased incidence of cancer after CT scan exposure in this cohort was mostly due to irradiation. In this group, one in every 1,800 CT scans was followed by an excess cancer. If the lifetime risk of developing cancer is 40% then the absolute risk rises to 40.05% after a CT.[141][142]
Some studies have shown that publications indicating an increased risk of cancer from typical doses of body CT scans are plagued with serious methodological limitations and several highly improbable results,[143] concluding that no evidence indicates such low doses cause any long-term harm.[144][145][146]
One study estimated that as many as 0.4% of cancers in the United States resulted from CT scans, and that this may have increased to as much as 1.5 to 2% based on the rate of CT use in 2007.[134] Others dispute this estimate,[147] as there is no consensus that the low levels of radiation used in CT scans cause damage. Lower radiation doses are used in many cases, such as in the investigation of renal colic.[148]
A person’s age plays a significant role in the subsequent risk of cancer.[149] Estimated lifetime cancer mortality risks from an abdominal CT of a one-year-old is 0.1%, or 1:1000 scans.[149] The risk for someone who is 40 years old is half that of someone who is 20 years old with substantially less risk in the elderly.[149] The International Commission on Radiological Protection estimates that the risk to a fetus being exposed to 10 mGy (a unit of radiation exposure) increases the rate of cancer before 20 years of age from 0.03% to 0.04% (for reference a CT pulmonary angiogram exposes a fetus to 4 mGy).[150] A 2012 review did not find an association between medical radiation and cancer risk in children noting however the existence of limitations in the evidences over which the review is based.[151]
CT scans can be performed with different settings for lower exposure in children with most manufacturers of CT scans as of 2007 having this function built in.[152] Furthermore, certain conditions can require children to be exposed to multiple CT scans.[134] Current evidence suggests informing parents of the risks of pediatric CT scanning.[153]
Contrast reactions[edit]
In the United States half of CT scans are contrast CTs using intravenously injected radiocontrast agents.[154] The most common reactions from these agents are mild, including nausea, vomiting, and an itching rash. Severe life-threatening reactions may rarely occur.[155] Overall reactions occur in 1 to 3% with nonionic contrast and 4 to 12% of people with ionic contrast.[156] Skin rashes may appear within a week to 3% of people.[155]
The old radiocontrast agents caused anaphylaxis in 1% of cases while the newer, low-osmolar agents cause reactions in 0.01–0.04% of cases.[155][157] Death occurs in about 2 to 30 people per 1,000,000 administrations, with newer agents being safer.[156][158]
There is a higher risk of mortality in those who are female, elderly or in poor health, usually secondary to either anaphylaxis or acute kidney injury.[154]
The contrast agent may induce contrast-induced nephropathy.[159] This occurs in 2 to 7% of people who receive these agents, with greater risk in those who have preexisting kidney failure,[159] preexisting diabetes, or reduced intravascular volume. People with mild kidney impairment are usually advised to ensure full hydration for several hours before and after the injection. For moderate kidney failure, the use of iodinated contrast should be avoided; this may mean using an alternative technique instead of CT. Those with severe kidney failure requiring dialysis require less strict precautions, as their kidneys have so little function remaining that any further damage would not be noticeable and the dialysis will remove the contrast agent; it is normally recommended, however, to arrange dialysis as soon as possible following contrast administration to minimize any adverse effects of the contrast.
In addition to the use of intravenous contrast, orally administered contrast agents are frequently used when examining the abdomen.[160] These are frequently the same as the intravenous contrast agents, merely diluted to approximately 10% of the concentration. However, oral alternatives to iodinated contrast exist, such as very dilute (0.5–1% w/v) barium sulfate suspensions. Dilute barium sulfate has the advantage that it does not cause allergic-type reactions or kidney failure, but cannot be used in patients with suspected bowel perforation or suspected bowel injury, as leakage of barium sulfate from damaged bowel can cause fatal peritonitis.[161]
Side effects from contrast agents, administered intravenously in some CT scans, might impair kidney performance in patients with kidney disease, although this risk is now believed to be lower than previously thought.[162][159]
Scan dose[edit]
| Examination | Typical effective dose (mSv) to the whole body |
Typical absorbed dose (mGy) to the organ in question |
|---|---|---|
| Annual background radiation | 2.4[163] | 2.4[163] |
| Chest X-ray | 0.02[164] | 0.01–0.15[165] |
| Head CT | 1–2[149] | 56[166] |
| Screening mammography | 0.4[150] | 3[134][165] |
| Abdominal CT | 8[164] | 14[166] |
| Chest CT | 5–7[149] | 13[166] |
| CT colonography | 6–11[149] | |
| Chest, abdomen and pelvis CT | 9.9[166] | 12[166] |
| Cardiac CT angiogram | 9–12[149] | 40–100[165] |
| Barium enema | 15[134] | 15[165] |
| Neonatal abdominal CT | 20[134] | 20[165] |
|
Further information: Template:Effective dose by medical imaging type |
The table reports average radiation exposures; however, there can be a wide variation in radiation doses between similar scan types, where the highest dose could be as much as 22 times higher than the lowest dose.[149] A typical plain film X-ray involves radiation dose of 0.01 to 0.15 mGy, while a typical CT can involve 10–20 mGy for specific organs, and can go up to 80 mGy for certain specialized CT scans.[165]
For purposes of comparison, the world average dose rate from naturally occurring sources of background radiation is 2.4 mSv per year, equal for practical purposes in this application to 2.4 mGy per year.[163] While there is some variation, most people (99%) received less than 7 mSv per year as background radiation.[167] Medical imaging as of 2007 accounted for half of the radiation exposure of those in the United States with CT scans making up two thirds of this amount.[149] In the United Kingdom it accounts for 15% of radiation exposure.[150] The average radiation dose from medical sources is ≈0.6 mSv per person globally as of 2007.[149] Those in the nuclear industry in the United States are limited to doses of 50 mSv a year and 100 mSv every 5 years.[149]
Lead is the main material used by radiography personnel for shielding against scattered X-rays.
Radiation dose units[edit]
The radiation dose reported in the gray or mGy unit is proportional to the amount of energy that the irradiated body part is expected to absorb, and the physical effect (such as DNA double strand breaks) on the cells’ chemical bonds by X-ray radiation is proportional to that energy.[168]
The sievert unit is used in the report of the effective dose. The sievert unit, in the context of CT scans, does not correspond to the actual radiation dose that the scanned body part absorbs but to another radiation dose of another scenario, the whole body absorbing the other radiation dose and the other radiation dose being of a magnitude, estimated to have the same probability to induce cancer as the CT scan.[169] Thus, as is shown in the table above, the actual radiation that is absorbed by a scanned body part is often much larger than the effective dose suggests. A specific measure, termed the computed tomography dose index (CTDI), is commonly used as an estimate of the radiation absorbed dose for tissue within the scan region, and is automatically computed by medical CT scanners.[170]
The equivalent dose is the effective dose of a case, in which the whole body would actually absorb the same radiation dose, and the sievert unit is used in its report. In the case of non-uniform radiation, or radiation given to only part of the body, which is common for CT examinations, using the local equivalent dose alone would overstate the biological risks to the entire organism.[171][172][173]
Effects of radiation[edit]
Most adverse health effects of radiation exposure may be grouped in two general categories:
- deterministic effects (harmful tissue reactions) due in large part to the killing/ malfunction of cells following high doses;[174]
- stochastic effects, i.e., cancer and heritable effects involving either cancer development in exposed individuals owing to mutation of somatic cells or heritable disease in their offspring owing to mutation of reproductive (germ) cells.[175]
The added lifetime risk of developing cancer by a single abdominal CT of 8 mSv is estimated to be 0.05%, or 1 one in 2,000.[176]
Because of increased susceptibility of fetuses to radiation exposure, the radiation dosage of a CT scan is an important consideration in the choice of medical imaging in pregnancy.[177][178]
Excess doses[edit]
In October, 2009, the US Food and Drug Administration (FDA) initiated an investigation of brain perfusion CT (PCT) scans, based on radiation burns caused by incorrect settings at one particular facility for this particular type of CT scan. Over 256 patients were exposed to radiations for over 18-month period. Over 40% of them lost patches of hair, and prompted the editorial to call for increased CT quality assurance programs. It was noted that «while unnecessary radiation exposure should be avoided, a medically needed CT scan obtained with appropriate acquisition parameter has benefits that outweigh the radiation risks.»[149][179] Similar problems have been reported at other centers.[149] These incidents are believed to be due to human error.[149]
Mechanism[edit]
CT scanner with cover removed to show internal components. Legend:
T: X-ray tube
D: X-ray detectors
X: X-ray beam
R: Gantry rotation
Left image is a sinogram which is a graphic representation of the raw data obtained from a CT scan. At right is an image sample derived from the raw data.[180]
Computed tomography operates by using an X-ray generator that rotates around the object; X-ray detectors are positioned on the opposite side of the circle from the X-ray source.[181] As the X-rays pass through the patient, they are attenuated differently by various tissues according to the tissue density.[182] A visual representation of the raw data obtained is called a sinogram, yet it is not sufficient for interpretation.[183] Once the scan data has been acquired, the data must be processed using a form of tomographic reconstruction, which produces a series of cross-sectional images.[184] These cross-sectional images are made up of small units of pixels or voxels.[185]
Pixels in an image obtained by CT scanning are displayed in terms of relative radiodensity. The pixel itself is displayed according to the mean attenuation of the tissue(s) that it corresponds to on a scale from +3,071 (most attenuating) to −1,024 (least attenuating) on the Hounsfield scale. A pixel is a two dimensional unit based on the matrix size and the field of view. When the CT slice thickness is also factored in, the unit is known as a voxel, which is a three-dimensional unit.[185]
Water has an attenuation of 0 Hounsfield units (HU), while air is −1,000 HU, cancellous bone is typically +400 HU, and cranial bone can reach 2,000 HU or more (os temporale) and can cause artifacts. The attenuation of metallic implants depends on the atomic number of the element used: Titanium usually has an amount of +1000 HU, iron steel can completely extinguish the X-ray and is, therefore, responsible for well-known line-artifacts in computed tomograms. Artifacts are caused by abrupt transitions between low- and high-density materials, which results in data values that exceed the dynamic range of the processing electronics. Two-dimensional CT images are conventionally rendered so that the view is as though looking up at it from the patient’s feet.[87] Hence, the left side of the image is to the patient’s right and vice versa, while anterior in the image also is the patient’s anterior and vice versa. This left-right interchange corresponds to the view that physicians generally have in reality when positioned in front of patients.
Initially, the images generated in CT scans were in the transverse (axial) anatomical plane, perpendicular to the long axis of the body. Modern scanners allow the scan data to be reformatted as images in other planes. Digital geometry processing can generate a three-dimensional image of an object inside the body from a series of two-dimensional radiographic images taken by rotation around a fixed axis.[110] These cross-sectional images are widely used for medical diagnosis and therapy.[186]
Contrast[edit]
Contrast media used for X-ray CT, as well as for plain film X-ray, are called radiocontrasts. Radiocontrasts for CT are, in general, iodine-based.[187] This is useful to highlight structures such as blood vessels that otherwise would be difficult to delineate from their surroundings. Using contrast material can also help to obtain functional information about tissues. Often, images are taken both with and without radiocontrast.[188]
History[edit]
The history of X-ray computed tomography goes back to at least 1917 with the mathematical theory of the Radon transform.[189][190] In October 1963, William H. Oldendorf received a U.S. patent for a «radiant energy apparatus for investigating selected areas of interior objects obscured by dense material».[191] The first commercially viable CT scanner was invented by Godfrey Hounsfield in 1972.[192]
Etymology[edit]
The word «tomography» is derived from the Greek tome (slice) and graphein (to write).[193] Computed tomography was originally known as the «EMI scan» as it was developed in the early 1970s at a research branch of EMI, a company best known today for its music and recording business.[194] It was later known as computed axial tomography (CAT or CT scan) and body section röntgenography.[195]
The term «CAT scan» is no longer used because current CT scans enable for multiplanar reconstructions. This makes «CT scan» the most appropriate term, which is used by radiologists in common vernacular as well as in textbooks and scientific papers.[196][197][198]
In Medical Subject Headings (MeSH), «computed axial tomography» was used from 1977 to 1979, but the current indexing explicitly includes «X-ray» in the title.[199]
The term sinogram was introduced by Paul Edholm and Bertil Jacobson in 1975.[200]
Society and culture[edit]
Campaigns[edit]
In response to increased concern by the public and the ongoing progress of best practices, the Alliance for Radiation Safety in Pediatric Imaging was formed within the Society for Pediatric Radiology. In concert with the American Society of Radiologic Technologists, the American College of Radiology and the American Association of Physicists in Medicine, the Society for Pediatric Radiology developed and launched the Image Gently Campaign which is designed to maintain high-quality imaging studies while using the lowest doses and best radiation safety practices available on pediatric patients.[201] This initiative has been endorsed and applied by a growing list of various professional medical organizations around the world and has received support and assistance from companies that manufacture equipment used in Radiology.
Following upon the success of the Image Gently campaign, the American College of Radiology, the Radiological Society of North America, the American Association of Physicists in Medicine and the American Society of Radiologic Technologists have launched a similar campaign to address this issue in the adult population called Image Wisely.[202]
The World Health Organization and International Atomic Energy Agency (IAEA) of the United Nations have also been working in this area and have ongoing projects designed to broaden best practices and lower patient radiation dose.[203][204]
Prevalence[edit]
Use of CT has increased dramatically over the last two decades.[19] An estimated 72 million scans were performed in the United States in 2007,[20] accounting for close to half of the total per-capita dose rate from radiologic and nuclear medicine procedures.[206] Of the CT scans, six to eleven percent are done in children,[150] an increase of seven to eightfold from 1980.[149] Similar increases have been seen in Europe and Asia.[149] In Calgary, Canada, 12.1% of people who present to the emergency with an urgent complaint received a CT scan, most commonly either of the head or of the abdomen. The percentage who received CT, however, varied markedly by the emergency physician who saw them from 1.8% to 25%.[207] In the emergency department in the United States, CT or MRI imaging is done in 15% of people who present with injuries as of 2007 (up from 6% in 1998).[208]
The increased use of CT scans has been the greatest in two fields: screening of adults (screening CT of the lung in smokers, virtual colonoscopy, CT cardiac screening, and whole-body CT in asymptomatic patients) and CT imaging of children. Shortening of the scanning time to around 1 second, eliminating the strict need for the subject to remain still or be sedated, is one of the main reasons for the large increase in the pediatric population (especially for the diagnosis of appendicitis).[134] As of 2007, in the United States a proportion of CT scans are performed unnecessarily.[152] Some estimates place this number at 30%.[150] There are a number of reasons for this including: legal concerns, financial incentives, and desire by the public.[152] For example, some healthy people avidly pay to receive full-body CT scans as screening. In that case, it is not at all clear that the benefits outweigh the risks and costs. Deciding whether and how to treat incidentalomas is complex, radiation exposure is not negligible, and the money for the scans involves opportunity cost.[152]
Manufacturers[edit]
Major manufacturers of CT Scanners Devices and Equipment are:[209]
Research[edit]
Photon-counting computed tomography is a CT technique currently under development. Typical CT scanners use energy integrating detectors; photons are measured as a voltage on a capacitor which is proportional to the x-rays detected. However, this technique is susceptible to noise and other factors which can affect the linearity of the voltage to x-ray intensity relationship.[210] Photon counting detectors (PCDs) are still affected by noise but it does not change the measured counts of photons. PCDs have several potential advantages, including improving signal (and contrast) to noise ratios, reducing doses, improving spatial resolution, and through use of several energies, distinguishing multiple contrast agents.[211][212] PCDs have only recently become feasible in CT scanners due to improvements in detector technologies that can cope with the volume and rate of data required. As of February 2016, photon counting CT is in use at three sites.[213] Some early research has found the dose reduction potential of photon counting CT for breast imaging to be very promising.[214] In view of recent findings of high cumulative doses to patients from recurrent CT scans, there has been a push for scanning technologies and techniques that reduce ionising radiation doses to patients to sub-milliSievert (sub-mSv in the literature) levels during the CT scan process, a goal that has been lingering.[215][138][139][140]
See also[edit]
- Barium sulfate suspension
- Dosimetry
- Tomosynthesis
- Virtopsy
- X-ray microtomography
- Xenon-enhanced CT scanning
References[edit]
- ^ «CT scan – Mayo Clinic». mayoclinic.org. Archived from the original on 15 October 2016. Retrieved 20 October 2016.
- ^ «Patient Page». ARRT – The American Registry of Radiologic Technologists. Archived from the original on 9 November 2014.
- ^ «Individual State Licensure Information». American Society of Radiologic Technologists. Archived from the original on 18 July 2013. Retrieved 19 July 2013.
- ^ «The Nobel Prize in Physiology or Medicine 1979». NobelPrize.org. Retrieved 2019-08-10.
- ^ Fishman, Elliot K.; Jeffrey, R. Brooke (1995). Spiral CT: Principles, Techniques, and Clinical Applications. Raven Press. ISBN 978-0-7817-0218-8.
- ^ Hsieh, Jiang (2003). Computed Tomography: Principles, Design, Artifacts, and Recent Advances. SPIE Press. p. 265. ISBN 978-0-8194-4425-7.
- ^ Stirrup, James (2020-01-02). Cardiovascular Computed Tomography. Oxford University Press. ISBN 978-0-19-880927-2.
- ^ Talisetti, Anita; Jelnin, Vladimir; Ruiz, Carlos; John, Eunice; Benedetti, Enrico; Testa, Giuliano; Holterman, Ai-Xuan L.; Holterman, Mark J. (December 2004). «Electron beam CT scan is a valuable and safe imaging tool for the pediatric surgical patient». Journal of Pediatric Surgery. 39 (12): 1859–1862. doi:10.1016/j.jpedsurg.2004.08.024. ISSN 1531-5037. PMID 15616951.
- ^ Retsky, Michael (31 July 2008). «Electron beam computed tomography: Challenges and opportunities». Physics Procedia. 1 (1): 149–154. Bibcode:2008PhPro…1..149R. doi:10.1016/j.phpro.2008.07.090.
- ^ Carrascosa, Patricia M.; Cury, Ricardo C.; García, Mario J.; Leipsic, Jonathon A. (2015-10-03). Dual-Energy CT in Cardiovascular Imaging. Springer. ISBN 978-3-319-21227-2.
- ^ Schmidt, Bernhard; Flohr, Thomas (2020-11-01). «Principles and applications of dual source CT». Physica Medica. 125 Years of X-Rays. 79: 36–46. doi:10.1016/j.ejmp.2020.10.014. ISSN 1120-1797. PMID 33115699. S2CID 226056088.
- ^ a b Seidensticker, Peter R.; Hofmann, Lars K. (2008-05-24). Dual Source CT Imaging. Springer Science & Business Media. ISBN 978-3-540-77602-4.
- ^ Schmidt, Bernhard; Flohr, Thomas (2020-11-01). «Principles and applications of dual source CT». Physica Medica: European Journal of Medical Physics. 79: 36–46. doi:10.1016/j.ejmp.2020.10.014. ISSN 1120-1797. PMID 33115699. S2CID 226056088.
- ^ a b c Wittsack, H.-J.; Wohlschläger, A.M.; Ritzl, E.K.; Kleiser, R.; Cohnen, M.; Seitz, R.J.; Mödder, U. (2008-01-01). «CT-perfusion imaging of the human brain: Advanced deconvolution analysis using circulant singular value decomposition». Computerized Medical Imaging and Graphics. 32 (1): 67–77. doi:10.1016/j.compmedimag.2007.09.004. ISSN 0895-6111. PMID 18029143.
- ^ Williams, M.C.; Newby, D.E. (2016-08-01). «CT myocardial perfusion imaging: current status and future directions». Clinical Radiology. 71 (8): 739–749. doi:10.1016/j.crad.2016.03.006. ISSN 0009-9260. PMID 27091433.
- ^ a b Donahue, Joseph; Wintermark, Max (2015-02-01). «Perfusion CT and acute stroke imaging: Foundations, applications, and literature review». Journal of Neuroradiology. 42 (1): 21–29. doi:10.1016/j.neurad.2014.11.003. ISSN 0150-9861. PMID 25636991.
- ^ Curry, Thomas S.; Dowdey, James E.; Murry, Robert C. (1990). Christensen’s Physics of Diagnostic Radiology. Lippincott Williams & Wilkins. p. 289. ISBN 978-0-8121-1310-5.
- ^ «CT Screening» (PDF). hps.org. Archived from the original (PDF) on 13 October 2016. Retrieved 1 May 2018.
- ^ a b Smith-Bindman R, Lipson J, Marcus R, Kim KP, Mahesh M, Gould R, Berrington de González A, Miglioretti DL (December 2009). «Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer». Arch. Intern. Med. 169 (22): 2078–86. doi:10.1001/archinternmed.2009.427. PMC 4635397. PMID 20008690.
- ^ a b Berrington de González A, Mahesh M, Kim KP, Bhargavan M, Lewis R, Mettler F, Land C (December 2009). «Projected cancer risks from computed tomographic scans performed in the United States in 2007». Arch. Intern. Med. 169 (22): 2071–7. doi:10.1001/archinternmed.2009.440. PMC 6276814. PMID 20008689.
- ^ «Dangers of CT Scans and X-Rays – Consumer Reports». Retrieved 16 May 2018.
- ^ Surgeons (AAOS), American Academy of Orthopaedic; Physicians (ACEP), American College of Emergency; UMBC (2017-03-20). Critical Care Transport. Jones & Bartlett Learning. p. 389. ISBN 978-1-284-04099-9.
- ^ Galloway, RL Jr. (2015). «Introduction and Historical Perspectives on Image-Guided Surgery». In Golby, AJ (ed.). Image-Guided Neurosurgery. Amsterdam: Elsevier. pp. 3–4. ISBN 978-0-12-800870-6.
- ^ Tse, VCK; Kalani, MYS; Adler, JR (2015). «Techniques of Stereotactic Localization». In Chin, LS; Regine, WF (eds.). Principles and Practice of Stereotactic Radiosurgery. New York: Springer. p. 28. ISBN 978-0-387-71070-9.
- ^ Saleh, H; Kassas, B (2015). «Developing Stereotactic Frames for Cranial Treatment». In Benedict, SH; Schlesinger, DJ; Goetsch, SJ; Kavanagh, BD (eds.). Stereotactic Radiosurgery and Stereotactic Body Radiation Therapy. Boca Raton: CRC Press. pp. 156–159. ISBN 978-1-4398-4198-3.
- ^ Khan, FR; Henderson, JM (2013). «Deep Brain Stimulation Surgical Techniques». In Lozano, AM; Hallet, M (eds.). Brain Stimulation. Handbook of Clinical Neurology. Vol. 116. Amsterdam: Elsevier. pp. 28–30. doi:10.1016/B978-0-444-53497-2.00003-6. ISBN 978-0-444-53497-2. PMID 24112882.
- ^ Arle, J (2009). «Development of a Classic: the Todd-Wells Apparatus, the BRW, and the CRW Stereotactic Frames». In Lozano, AM; Gildenberg, PL; Tasker, RR (eds.). Textbook of Stereotactic and Functional Neurosurgery. Berlin: Springer-Verlag. pp. 456–461. ISBN 978-3-540-69959-0.
- ^ Brown RA, Nelson JA (June 2012). «Invention of the N-localizer for stereotactic neurosurgery and its use in the Brown-Roberts-Wells stereotactic frame». Neurosurgery. 70 (2 Supplement Operative): 173–176. doi:10.1227/NEU.0b013e318246a4f7. PMID 22186842. S2CID 36350612.
- ^ Daniel G Deschler, Joseph Zenga. «Evaluation of a neck mass in adults». UpToDate. This topic last updated: Dec 04, 2017.
- ^ a b Bin Saeedan, Mnahi; Aljohani, Ibtisam Musallam; Khushaim, Ayman Omar; Bukhari, Salwa Qasim; Elnaas, Salahudin Tayeb (2016). «Thyroid computed tomography imaging: pictorial review of variable pathologies». Insights into Imaging. 7 (4): 601–617. doi:10.1007/s13244-016-0506-5. ISSN 1869-4101. PMC 4956631. PMID 27271508.
- ^ Computed Tomography of the Lung. Springer Berlin Heidelberg. 2007. pp. 40, 47. ISBN 978-3-642-39518-5.
- ^ High-resolution CT of the Lung. Lippincott Williams & Wilkins. 2009. pp. 81, 568. ISBN 978-0-7817-6909-9.
- ^ Martínez-Jiménez, Santiago; Rosado-de-Christenson, Melissa L.; Carter, Brett W. (2017-07-22). Specialty Imaging: HRCT of the Lung E-Book. Elsevier Health Sciences. ISBN 978-0-323-52495-7.
- ^ Yuranga Weerakkody. «Bronchial wall thickening». Radiopaedia. Archived from the original on 2018-01-06. Retrieved 2018-01-05.
- ^ Wiener RS, Gould MK, Woloshin S, Schwartz LM, Clark JA (2012). ««What do you mean, a spot?»: A qualitative analysis of patients’ reactions to discussions with their doctors about pulmonary nodules». Chest. 143 (3): 672–677. doi:10.1378/chest.12-1095. PMC 3590883. PMID 22814873.
- ^ a b c American College of Chest Physicians; American Thoracic Society (September 2013), «Five Things Physicians and Patients Should Question», Choosing Wisely, American College of Chest Physicians and American Thoracic Society, archived from the original on 3 November 2013, retrieved 6 January 2013, which cites
- MacMahon H, Austin JH, Gamsu G, Herold CJ, Jett JR, Naidich DP, Patz EF, Swensen SJ (2005). «Guidelines for Management of Small Pulmonary Nodules Detected on CT Scans: A Statement from the Fleischner Society1». Radiology. 237 (2): 395–400. doi:10.1148/radiol.2372041887. PMID 16244247. S2CID 14498160.
- Gould MK, Fletcher J, Iannettoni MD, Lynch WR, Midthun DE, Naidich DP, Ost DE (2007). «Evaluation of Patients with Pulmonary Nodules: When is It Lung Cancer?*». Chest. 132 (3_suppl): 108S–130S. doi:10.1378/chest.07-1353. PMID 17873164. S2CID 16449420.
- Smith-Bindman R, Lipson J, Marcus R, Kim KP, Mahesh M, Gould R, Berrington de González A, Miglioretti DL (2009). «Radiation Dose Associated with Common Computed Tomography Examinations and the Associated Lifetime Attributable Risk of Cancer». Archives of Internal Medicine. 169 (22): 2078–2086. doi:10.1001/archinternmed.2009.427. PMC 4635397. PMID 20008690.
- Wiener RS, Gould MK, Woloshin S, Schwartz LM, Clark JA (2012). ««What do you mean, a spot?»: A qualitative analysis of patients’ reactions to discussions with their doctors about pulmonary nodules». Chest. 143 (3): 672–677. doi:10.1378/chest.12-1095. PMC 3590883. PMID 22814873.
- ^ McDermott, M.; Jacobs, T.; Morgenstern, L. (2017-01-01), Wijdicks, Eelco F. M.; Kramer, Andreas H. (eds.), «Chapter 10 – Critical care in acute ischemic stroke», Handbook of Clinical Neurology, Critical Care Neurology Part I, Elsevier, 140: 153–176, doi:10.1016/b978-0-444-63600-3.00010-6, PMID 28187798
- ^ «Computed Tomography Angiography (CTA)». www.hopkinsmedicine.org. 19 November 2019. Retrieved 2021-03-21.
- ^ Zeman, R K; Silverman, P M; Vieco, P T; Costello, P (1995-11-01). «CT angiography». American Journal of Roentgenology. 165 (5): 1079–1088. doi:10.2214/ajr.165.5.7572481. ISSN 0361-803X. PMID 7572481.
- ^ Ramalho, Joana; Castillo, Mauricio (2014-03-31). Vascular Imaging of the Central Nervous System: Physical Principles, Clinical Applications, and Emerging Techniques. John Wiley & Sons. p. 69. ISBN 978-1-118-18875-0.
- ^ «Cardiac CT Scan – NHLBI, NIH». www.nhlbi.nih.gov. Archived from the original on 2017-12-01. Retrieved 2017-11-22.
- ^ a b Wichmann, Julian L. «Cardiac CT | Radiology Reference Article | Radiopaedia.org». radiopaedia.org. Archived from the original on 2017-12-01. Retrieved 2017-11-22.
- ^ Marwan, Mohamed; Achenbach, Stephan (February 2016). «Role of Cardiac CT Before Transcatheter Aortic Valve Implantation (TAVI)». Current Cardiology Reports. 18 (2): 21. doi:10.1007/s11886-015-0696-3. ISSN 1534-3170. PMID 26820560. S2CID 41535442.
- ^ Moss, Alastair J.; Dweck, Marc R.; Dreisbach, John G.; Williams, Michelle C.; Mak, Sze Mun; Cartlidge, Timothy; Nicol, Edward D.; Morgan-Hughes, Gareth J. (2016-11-01). «Complementary role of cardiac CT in the assessment of aortic valve replacement dysfunction». Open Heart. 3 (2): e000494. doi:10.1136/openhrt-2016-000494. ISSN 2053-3624. PMC 5093391. PMID 27843568.
- ^ Thériault-Lauzier, Pascal; Spaziano, Marco; Vaquerizo, Beatriz; Buithieu, Jean; Martucci, Giuseppe; Piazza, Nicolo (September 2015). «Computed Tomography for Structural Heart Disease and Interventions». Interventional Cardiology Review. 10 (3): 149–154. doi:10.15420/ICR.2015.10.03.149. ISSN 1756-1477. PMC 5808729. PMID 29588693.
- ^ Passariello, Roberto (2006-03-30). Multidetector-Row CT Angiography. Springer Science & Business Media. ISBN 978-3-540-26984-7.
- ^ Radiology (ACR), Radiological Society of North America (RSNA) and American College of. «Coronary Computed Tomography Angiography (CCTA)». www.radiologyinfo.org. Retrieved 2021-03-19.
- ^ «Heart scan (coronary calcium scan)». Mayo Clinic. Archived from the original on 5 September 2015. Retrieved 9 August 2015.
- ^ van der Bijl, Noortje; Joemai, Raoul M. S.; Geleijns, Jacob; Bax, Jeroen J.; Schuijf, Joanne D.; de Roos, Albert; Kroft, Lucia J. M. (2010). «Assessment of Agatston Coronary Artery Calcium Score Using Contrast-Enhanced CT Coronary Angiography». American Journal of Roentgenology. 195 (6): 1299–1305. doi:10.2214/AJR.09.3734. ISSN 0361-803X. PMID 21098187.
- ^ Vukicevic, Marija; Mosadegh, Bobak; Min, James K.; Little, Stephen H. (February 2017). «Cardiac 3D Printing and its Future Directions». JACC: Cardiovascular Imaging. 10 (2): 171–184. doi:10.1016/j.jcmg.2016.12.001. ISSN 1876-7591. PMC 5664227. PMID 28183437.
- ^ Wang, D. D.; Eng, M.; Greenbaum, A.; Myers, E.; Forbes, M.; Pantelic, M.; Song, T.; Nelson, C.; Divine, G.; Taylor, A.; Wyman, J.; Guerrero, M.; Lederman, R. J.; Paone, G.; O’Neill, W. (2016). «Innovative Mitral Valve Treatment with 3D Visualization at Henry Ford». JACC: Cardiovascular Imaging. 9 (11): 1349–1352. doi:10.1016/j.jcmg.2016.01.017. PMC 5106323. PMID 27209112. Archived from the original on 2017-12-01. Retrieved 2017-11-22.
- ^ Wang, Dee Dee; Eng, Marvin; Greenbaum, Adam; Myers, Eric; Forbes, Michael; Pantelic, Milan; Song, Thomas; Nelson, Christina; Divine, George (November 2016). «Predicting LVOT Obstruction After TMVR». JACC: Cardiovascular Imaging. 9 (11): 1349–1352. doi:10.1016/j.jcmg.2016.01.017. ISSN 1876-7591. PMC 5106323. PMID 27209112.
- ^ Jacobs, Stephan; Grunert, Ronny; Mohr, Friedrich W.; Falk, Volkmar (February 2008). «3D-Imaging of cardiac structures using 3D heart models for planning in heart surgery: a preliminary study». Interactive Cardiovascular and Thoracic Surgery. 7 (1): 6–9. doi:10.1510/icvts.2007.156588. ISSN 1569-9285. PMID 17925319.
- ^ Furukawa, Akira; Saotome, Takao; Yamasaki, Michio; Maeda, Kiyosumi; Nitta, Norihisa; Takahashi, Masashi; Tsujikawa, Tomoyuki; Fujiyama, Yoshihide; Murata, Kiyoshi; Sakamoto, Tsutomu (2004-05-01). «Cross-sectional Imaging in Crohn Disease». RadioGraphics. 24 (3): 689–702. doi:10.1148/rg.243035120. ISSN 0271-5333. PMID 15143222.
- ^ CT of the Acute Abdomen. Springer Berlin Heidelberg. 2011. p. 37. ISBN 978-3-540-89232-8.
- ^ Jay P Heiken; Douglas S Katz (2014). «Emergency Radiology of the Abdomen and Pelvis: Imaging of the Nontraumatic and Traumatic Acute Abdomen». In J. Hodler; R. A. Kubik-Huch; G. K. von Schulthess; Ch. L. Zollikofer (eds.). Diseases of the Abdomen and Pelvis. Springer Milan. p. 3. ISBN 9788847056596.
- ^ Skolarikos, A; Neisius, A; Petřík, A; Somani, B; Thomas, K; Gambaro, G (March 2022). EAU Guidelines on Urolithiasis. Amsterdam: European Association of Urology. ISBN 978-94-92671-16-5.
- ^ Miller, Oren F.; Kane, Christopher J. (September 1999). «Time to stone passage for observed ureteral calculi: a guide for patient education». Journal of Urology. 162 (3 Part 1): 688–691. doi:10.1097/00005392-199909010-00014. PMID 10458343.
- ^ «Ankle Fractures». orthoinfo.aaos.org. American Association of Orthopedic Surgeons. Archived from the original on 30 May 2010. Retrieved 30 May 2010.
- ^ Buckwalter, Kenneth A.; et al. (11 September 2000). «Musculoskeletal Imaging with Multislice CT». American Journal of Roentgenology. 176 (4): 979–986. doi:10.2214/ajr.176.4.1760979. PMID 11264094.
- ^ Ramon, André; Bohm-Sigrand, Amélie; Pottecher, Pierre; Richette, Pascal; Maillefert, Jean-Francis; Devilliers, Herve; Ornetti, Paul (2018-03-01). «Role of dual-energy CT in the diagnosis and follow-up of gout: systematic analysis of the literature». Clinical Rheumatology. 37 (3): 587–595. doi:10.1007/s10067-017-3976-z. ISSN 0770-3198. PMID 29350330. S2CID 3686099.
- ^ Keaveny, Tony M. (March 2010). «Biomechanical computed tomography-noninvasive bone strength analysis using clinical computed tomography scans». Annals of the New York Academy of Sciences. 1192 (1): 57–65. Bibcode:2010NYASA1192…57K. doi:10.1111/j.1749-6632.2009.05348.x. ISSN 1749-6632. PMID 20392218. S2CID 24132358.
- ^ Barber, Asa; Tozzi, Gianluca; Pani, Martino (2019-03-07). Computed Tomography Based Biomechanics. Frontiers Media SA. p. 20. ISBN 978-2-88945-780-9.
- ^ Evans, Ll. M.; Margetts, L.; Casalegno, V.; Lever, L. M.; Bushell, J.; Lowe, T.; Wallwork, A.; Young, P.; Lindemann, A. (2015-05-28). «Transient thermal finite element analysis of CFC–Cu ITER monoblock using X-ray tomography data». Fusion Engineering and Design. 100: 100–111. doi:10.1016/j.fusengdes.2015.04.048. Archived from the original on 2015-10-16.
- ^ Payne, Emma Marie (2012). «Imaging Techniques in Conservation» (PDF). Journal of Conservation and Museum Studies. 10 (2): 17–29. doi:10.5334/jcms.1021201.
- ^ P. Babaheidarian; D. Castanon (2018). «Joint reconstruction and material classification in spectral CT». Anomaly Detection and Imaging with X-Rays (ADIX) III. p. 12. doi:10.1117/12.2309663. ISBN 978-1-5106-1775-9. S2CID 65469251.
- ^ P. Jin; E. Haneda; K. D. Sauer; C. A. Bouman (June 2012). «A model-based 3D multi-slice helical CT reconstruction algorithm for transportation security application» (PDF). Second International Conference on Image Formation in X-Ray Computed Tomography. Archived from the original (PDF) on 2015-04-11. Retrieved 2015-04-05.
- ^ P. Jin; E. Haneda; C. A. Bouman (November 2012). «Implicit Gibbs prior models for tomographic reconstruction» (PDF). Signals, Systems and Computers (ASILOMAR), 2012 Conference Record of the Forty Sixth Asilomar Conference on. IEEE. pp. 613–636. Archived from the original (PDF) on 2015-04-11. Retrieved 2015-04-05.
- ^ S. J. Kisner; P. Jin; C. A. Bouman; K. D. Sauer; W. Garms; T. Gable; S. Oh; M. Merzbacher; S. Skatter (October 2013). «Innovative data weighting for iterative reconstruction in a helical CT security baggage scanner» (PDF). Security Technology (ICCST), 2013 47th International Carnahan Conference on. IEEE. Archived from the original (PDF) on 2015-04-10. Retrieved 2015-04-05.
- ^ Megherbi, N.; Flitton, G.T.; Breckon, T.P. (September 2010). «A Classifier based Approach for the Detection of Potential Threats in CT based Baggage Screening» (PDF). Proc. International Conference on Image Processing. IEEE. pp. 1833–1836. CiteSeerX 10.1.1.188.5206. doi:10.1109/ICIP.2010.5653676. ISBN 978-1-4244-7992-4. S2CID 3679917. Retrieved 5 November 2013.
- ^ Megherbi, N.; Han, J.; Flitton, G.T.; Breckon, T.P. (September 2012). «A Comparison of Classification Approaches for Threat Detection in CT based Baggage Screening» (PDF). Proc. International Conference on Image Processing. IEEE. pp. 3109–3112. CiteSeerX 10.1.1.391.2695. doi:10.1109/ICIP.2012.6467558. ISBN 978-1-4673-2533-2. S2CID 6924816. Retrieved 5 November 2013.
- ^ Flitton, G.T.; Breckon, T.P.; Megherbi, N. (September 2013). «A Comparison of 3D Interest Point Descriptors with Application to Airport Baggage Object Detection in Complex CT Imagery» (PDF). Pattern Recognition. 46 (9): 2420–2436. Bibcode:2013PatRe..46.2420F. doi:10.1016/j.patcog.2013.02.008. hdl:1826/15213. Retrieved 5 November 2013.
- ^ Russell, Molly (30 March 2022). «How Next Generation Airport Scanners Are Ending The 100ml Liquid Rule». Simple Flying. Simple Flying. Retrieved 11 April 2022.
- ^ «Laboratory | About Chikyu | The Deep-sea Scientific Drilling Vessel CHIKYU». www.jamstec.go.jp. Retrieved 2019-10-24.
- ^ Tonai, Satoshi; Kubo, Yusuke; Tsang, Man-Yin; Bowden, Stephen; Ide, Kotaro; Hirose, Takehiro; Kamiya, Nana; Yamamoto, Yuzuru; Yang, Kiho; Yamada, Yasuhiro; Morono, Yuki (2019). «A New Method for Quality Control of Geological Cores by X-Ray Computed Tomography: Application in IODP Expedition 370». Frontiers in Earth Science. 7. doi:10.3389/feart.2019.00117. ISSN 2296-6463. S2CID 171394807.
- ^ Seales, W. B.; Parker, C. S.; Segal, M.; Tov, E.; Shor, P.; Porath, Y. (2016). «From damage to discovery via virtual unwrapping: Reading the scroll from En-Gedi». Science Advances. 2 (9): e1601247. Bibcode:2016SciA….2E1247S. doi:10.1126/sciadv.1601247. ISSN 2375-2548. PMC 5031465. PMID 27679821.
- ^ Castellanos, Sara (2 March 2021). «A Letter Sealed for Centuries Has Been Read—Without Even Opening It». The Wall Street Journal. Retrieved 2 March 2021.
- ^ Dambrogio, Jana; Ghassaei, Amanda; Staraza Smith, Daniel; Jackson, Holly; Demaine, Martin L. (2 March 2021). «Unlocking history through automated virtual unfolding of sealed documents imaged by X-ray microtomography». Nature Communications. 12 (1): 1184. Bibcode:2021NatCo..12.1184D. doi:10.1038/s41467-021-21326-w. PMC 7925573. PMID 33654094.
- ^ Advanced documentation methods in studying Corinthian black-figure vase painting on YouTube showing a Computed Tomography scan and rollout of the aryballos No. G26, archaeological collection, Graz University. The video was rendered using the GigaMesh Software Framework, cf. doi:10.11588/heidok.00025189.
Karl, Stephan; Bayer, Paul; Mara, Hubert; Márton, András (2019), «Advanced Documentation Methods in Studying Corinthian Black-figure Vase Painting» (PDF), Proceedings of the 23rd International Conference on Cultural Heritage and New Technologies (CHNT23), Vienna, Austria, ISBN 978-3-200-06576-5, retrieved 2020-01-09 - ^ Bulcke, Jan Van den; Boone, Matthieu; Acker, Joris Van; Hoorebeke, Luc Van (October 2009). «Three-Dimensional X-Ray Imaging and Analysis of Fungi on and in Wood». Microscopy and Microanalysis. 15 (5): 395–402. Bibcode:2009MiMic..15..395V. doi:10.1017/S1431927609990419. hdl:1854/LU-675607. ISSN 1435-8115. PMID 19709462. S2CID 15637414.
- ^ Goldman, L. W. (2008). «Principles of CT: Multislice CT». Journal of Nuclear Medicine Technology. 36 (2): 57–68. doi:10.2967/jnmt.107.044826. ISSN 0091-4916. PMID 18483143.
- ^ a b Reis, Eduardo Pontes; Nascimento, Felipe; Aranha, Mateus; Mainetti Secol, Fernando; Machado, Birajara; Felix, Marcelo; Stein, Anouk; Amaro, Edson (29 July 2020). «Brain Hemorrhage Extended (BHX): Bounding box extrapolation from thick to thin slice CT images v1.1». PhysioNet. 101 (23): 215–220. doi:10.13026/9cft-hg92.
- ^ Park, S.; Chu, L.C.; Hruban, R.H.; Vogelstein, B.; Kinzler, K.W.; Yuille, A.L.; Fouladi, D.F.; Shayesteh, S.; Ghandili, S.; Wolfgang, C.L.; Burkhart, R.; He, J.; Fishman, E.K.; Kawamoto, S. (2020-09-01). «Differentiating autoimmune pancreatitis from pancreatic ductal adenocarcinoma with CT radiomics features». Diagnostic and Interventional Imaging. 101 (9): 555–564. doi:10.1016/j.diii.2020.03.002. ISSN 2211-5684. PMID 32278586. S2CID 215751181.
- ^ a b Fishman, Elliot K.; Ney, Derek R.; Heath, David G.; Corl, Frank M.; Horton, Karen M.; Johnson, Pamela T. (2006). «Volume Rendering versus Maximum Intensity Projection in CT Angiography: What Works Best, When, and Why». RadioGraphics. 26 (3): 905–922. doi:10.1148/rg.263055186. ISSN 0271-5333. PMID 16702462.
- ^ Silverstein, Jonathan C.; Parsad, Nigel M.; Tsirline, Victor (2008). «Automatic perceptual color map generation for realistic volume visualization». Journal of Biomedical Informatics. 41 (6): 927–935. doi:10.1016/j.jbi.2008.02.008. ISSN 1532-0464. PMC 2651027. PMID 18430609.
- ^ Kobbelt, Leif (2006). Vision, Modeling, and Visualization 2006: Proceedings, November 22-24, 2006, Aachen, Germany. IOS Press. p. 185. ISBN 978-3-89838-081-2.
- ^ a b Computerized Tomography chapter Archived 2016-03-04 at the Wayback Machine at University of Connecticut Health Center.
- ^ Schmidt, Derek; Odland, Rick (September 2004). «Mirror-Image Reversal of Coronal Computed Tomography Scans». The Laryngoscope. 114 (9): 1562–1565. doi:10.1097/00005537-200409000-00011. ISSN 0023-852X. PMID 15475782. S2CID 22320649.
- ^ Brant and Helms’ fundamentals of diagnostic radiology (Fifth ed.). Lippincott Williams & Wilkins. 2018-07-19. p. 1600. ISBN 978-1-4963-6738-9. Retrieved 24 January 2019.
- ^ Arthur W. Toga; John C. Mazziotta, eds. (2002). Brain mapping: the methods (2nd ed.). Amsterdam: Academic Press. ISBN 0-12-693019-8. OCLC 52594824.
- ^ Jerrold T. Bushberg; J. Anthony Seibert; Edwin M. Leidholdt; John M. Boone (2002). The essential physics of medical imaging (2nd ed.). Philadelphia: Lippincott Williams & Wilkins. p. 358. ISBN 0-683-30118-7. OCLC 47177732.
- ^ Kamalian, Shervin; Lev, Michael H.; Gupta, Rajiv (2016-01-01). «Computed tomography imaging and angiography – principles». Handbook of Clinical Neurology. 135: 3–20. doi:10.1016/B978-0-444-53485-9.00001-5. ISBN 978-0-444-53485-9. ISSN 0072-9752. PMID 27432657.
- ^ Stirrup, James (2020-01-02). Cardiovascular Computed Tomography. Oxford University Press. p. 136. ISBN 978-0-19-880927-2.
- ^ Udupa, Jayaram K.; Herman, Gabor T. (1999-09-28). 3D Imaging in Medicine, Second Edition. CRC Press. ISBN 978-0-8493-3179-4.
- ^ Krupski, Witold; Kurys-Denis, Ewa; Matuszewski, Łukasz; Plezia, Bogusław (2007-06-30). «Use of multi-planar reconstruction (MPR) and 3-dimentional [sic] (3D) CT to assess stability criteria in C2 vertebral fractures». Journal of Pre-Clinical and Clinical Research. 1 (1): 80–83. ISSN 1898-2395.
- ^ Tins, Bernhard (2010-10-21). «Technical aspects of CT imaging of the spine». Insights into Imaging. 1 (5–6): 349–359. doi:10.1007/s13244-010-0047-2. ISSN 1869-4101. PMC 3259341. PMID 22347928.
- ^ «CT imaging: Where are we going? (Proceedings)». DVM 360. Retrieved 2021-03-21.
- ^ Wolfson, Nikolaj; Lerner, Alexander; Roshal, Leonid (2016-05-30). Orthopedics in Disasters: Orthopedic Injuries in Natural Disasters and Mass Casualty Events. Springer. ISBN 978-3-662-48950-5.
- ^ Laroia, Archana T; Thompson, Brad H; Laroia, Sandeep T; van Beek, Edwin JR (2010-07-28). «Modern imaging of the tracheo-bronchial tree». World Journal of Radiology. 2 (7): 237–248. doi:10.4329/wjr.v2.i7.237. ISSN 1949-8470. PMC 2998855. PMID 21160663.
- ^ Gong, Jing-Shan; Xu, Jian-Min (2004-07-01). «Role of curved planar reformations using multidetector spiral CT in diagnosis of pancreatic and peripancreatic diseases». World Journal of Gastroenterology. 10 (13): 1943–1947. doi:10.3748/wjg.v10.i13.1943. ISSN 1007-9327. PMC 4572236. PMID 15222042.
- ^ Dalrymple, Neal C.; Prasad, Srinivasa R.; Freckleton, Michael W.; Chintapalli, Kedar N. (September 2005). «Informatics in radiology (infoRAD): introduction to the language of three-dimensional imaging with multidetector CT». Radiographics. 25 (5): 1409–1428. doi:10.1148/rg.255055044. ISSN 1527-1323. PMID 16160120.
- ^ Calhoun, Paul S.; Kuszyk, Brian S.; Heath, David G.; Carley, Jennifer C.; Fishman, Elliot K. (1999-05-01). «Three-dimensional Volume Rendering of Spiral CT Data: Theory and Method». RadioGraphics. 19 (3): 745–764. doi:10.1148/radiographics.19.3.g99ma14745. ISSN 0271-5333. PMID 10336201.
- ^ van Ooijen, P. M. A.; van Geuns, R. J. M.; Rensing, B. J. W. M.; Bongaerts, A. H. H.; de Feyter, P. J.; Oudkerk, M. (January 2003). «Noninvasive Coronary Imaging Using Electron Beam CT: Surface Rendering Versus Volume Rendering». American Journal of Roentgenology. 180 (1): 223–226. doi:10.2214/ajr.180.1.1800223. ISSN 0361-803X. PMID 12490509.
- ^ R. A. Crowther; D. J. DeRosier; A. Klug (1970). «The Reconstruction of a Three-Dimensional Structure from Projections and its Application to Electron Microscopy». Proc. R. Soc. Lond. A. 317 (1530): 319–340. Bibcode:1970RSPSA.317..319C. doi:10.1098/rspa.1970.0119. S2CID 122980366.
- ^ Nickoloff, Edward L.; Alderson, Philip O. (August 2001). «Radiation Exposures to Patients from CT: Reality, Public Perception, and Policy». American Journal of Roentgenology. 177 (2): 285–287. doi:10.2214/ajr.177.2.1770285. ISSN 0361-803X. PMID 11461846.
- ^ Barkan, O; Weill, J; Averbuch, A; Dekel, S. «Adaptive Compressed Tomography Sensing» Archived 2016-03-13 at the Wayback Machine. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition 2013 (pp. 2195–2202).
- ^ Proceedings. IEEE. 1995. p. 10. ISBN 9780780324985.
- ^ «Radiation – Effects on organs of the body (somatic effects)». Encyclopedia Britannica. Retrieved 2021-03-21.
- ^ Simpson G (2009). «Thoracic computed tomography: principles and practice». Australian Prescriber. 32 (4): 4. doi:10.18773/austprescr.2009.049.
- ^ a b Hsieh, Jiang (2003). Computed Tomography: Principles, Design, Artifacts, and Recent Advances. SPIE Press. p. 167. ISBN 978-0-8194-4425-7.
- ^ Bhowmik, Ujjal Kumar; Zafar Iqbal, M.; Adhami, Reza R. (28 May 2012). «Mitigating motion artifacts in FDK based 3D Cone-beam Brain Imaging System using markers». Central European Journal of Engineering. 2 (3): 369–382. Bibcode:2012CEJE….2..369B. doi:10.2478/s13531-012-0011-7.
- ^ a b P. Jin; C. A. Bouman; K. D. Sauer (2013). «A Method for Simultaneous Image Reconstruction and Beam Hardening Correction» (PDF). IEEE Nuclear Science Symp. & Medical Imaging Conf., Seoul, Korea, 2013. Archived from the original (PDF) on 2014-06-06. Retrieved 2014-04-23.
- ^ Boas FE, Fleischmann D (2011). «Evaluation of Two Iterative Techniques for Reducing Metal Artifacts in Computed Tomography». Radiology. 259 (3): 894–902. doi:10.1148/radiol.11101782. PMID 21357521.
- ^ Mouton, A.; Megherbi, N.; Van Slambrouck, K.; Nuyts, J.; Breckon, T.P. (2013). «An Experimental Survey of Metal Artefact Reduction in Computed Tomography» (PDF). Journal of X-Ray Science and Technology. 21 (2): 193–226. doi:10.3233/XST-130372. hdl:1826/8204. PMID 23694911.
- ^ Pessis, Eric; Campagna, Raphaël; Sverzut, Jean-Michel; Bach, Fabienne; Rodallec, Mathieu; Guerini, Henri; Feydy, Antoine; Drapé, Jean-Luc (2013). «Virtual Monochromatic Spectral Imaging with Fast Kilovoltage Switching: Reduction of Metal Artifacts at CT». RadioGraphics. 33 (2): 573–583. doi:10.1148/rg.332125124. ISSN 0271-5333. PMID 23479714.
- ^ González Ballester, Miguel Angel; Zisserman, Andrew P.; Brady, Michael (December 2002). «Estimation of the partial volume effect in MRI». Medical Image Analysis. 6 (4): 389–405. doi:10.1016/s1361-8415(02)00061-0. ISSN 1361-8415. PMID 12494949.
- ^ Goldszal, Alberto F.; Pham, Dzung L. (2000-01-01). «Volumetric Segmentation». Handbook of Medical Imaging: 185–194. doi:10.1016/B978-012077790-7/50016-3. ISBN 978-0-12-077790-7.
- ^ a b Jha, Diwaker (2014). «Adaptive center determination for effective suppression of ring artifacts in tomography images». Applied Physics Letters. 105 (14): 143107. Bibcode:2014ApPhL.105n3107J. doi:10.1063/1.4897441.
- ^ Van Nieuwenhove, V; De Beenhouwer, J; De Carlo, F; Mancini, L; Marone, F; Sijbers, J (2015). «Dynamic intensity normalization using eigen flat fields in X-ray imaging» (PDF). Optics Express. 23 (21): 27975–27989. Bibcode:2015OExpr..2327975V. doi:10.1364/oe.23.027975. hdl:10067/1302930151162165141. PMID 26480456.
- ^ Sijbers J, Postnov A (2004). «Reduction of ring artefacts in high resolution micro-CT reconstructions». Phys Med Biol. 49 (14): N247–53. doi:10.1088/0031-9155/49/14/N06. PMID 15357205. S2CID 12744174.
- ^ Newton, Thomas H.; Potts, D. Gordon (1971). Radiology of the Skull and Brain: Technical aspects of computed tomography. Mosby. pp. 3941–3950. ISBN 978-0-8016-3662-2.
- ^ Brüning, R.; Küttner, A.; Flohr, T. (2006-01-16). Protocols for Multislice CT. Springer Science & Business Media. ISBN 978-3-540-27273-1.
- ^ Peh, Wilfred C. G. (2017-08-11). Pitfalls in Musculoskeletal Radiology. Springer. ISBN 978-3-319-53496-1.
- ^ Van de Casteele E, Van Dyck D, Sijbers J, Raman E (2004). «A model-based correction method for beam hardening artefacts in X-ray microtomography». Journal of X-ray Science and Technology. 12 (1): 43–57. CiteSeerX 10.1.1.460.6487.
- ^ Van Gompel G, Van Slambrouck K, Defrise M, Batenburg KJ, Sijbers J, Nuyts J (2011). «Iterative correction of beam hardening artifacts in CT». Medical Physics. 38 (1): 36–49. Bibcode:2011MedPh..38S..36V. CiteSeerX 10.1.1.464.3547. doi:10.1118/1.3577758. PMID 21978116.
- ^ Mikla, Victor I.; Mikla, Victor V. (2013-08-23). Medical Imaging Technology. Elsevier. p. 37. ISBN 978-0-12-417036-0.
- ^ Radiology for the Dental Professional. Elsevier Mosby. 2008. p. 337. ISBN 978-0-323-03071-7.
- ^ Pasipoularides, Ares (November 2009). Heart’s Vortex: Intracardiac Blood Flow Phenomena. PMPH-USA. p. 595. ISBN 978-1-60795-033-2.
- ^ Heiken, JP; Peterson CM; Menias CO (November 2005). «Virtual colonoscopy for colorectal cancer screening: current status: Wednesday 5 October 2005, 14:00–16:00». Cancer Imaging. International Cancer Imaging Society. 5 (Spec No A): S133–S139. doi:10.1102/1470-7330.2005.0108. PMC 1665314. PMID 16361129.
- ^ Bielen DJ, Bosmans HT, De Wever LL, et al. (September 2005). «Clinical validation of high-resolution fast spin-echo MR colonography after colon distention with air». J Magn Reson Imaging. 22 (3): 400–5. doi:10.1002/jmri.20397. PMID 16106357. S2CID 22167728.
- ^ «CT Colonography». Radiologyinfo.org.
- ^ Žabić S, Wang Q, Morton T, Brown KM (March 2013). «A low dose simulation tool for CT systems with energy integrating detectors». Medical Physics. 40 (3): 031102. Bibcode:2013MedPh..40c1102Z. doi:10.1118/1.4789628. PMID 23464282.
- ^ Brian R. Subach M.D., F.A.C.S et al.»Reliability and accuracy of fine-cut computed tomography scans to determine the status of anterior interbody fusions with metallic cages» Archived 2012-12-08 at the Wayback Machine
- ^ a b c d e f g h Brenner DJ, Hall EJ (November 2007). «Computed tomography – an increasing source of radiation exposure» (PDF). N. Engl. J. Med. 357 (22): 2277–84. doi:10.1056/NEJMra072149. PMID 18046031. S2CID 2760372. Archived (PDF) from the original on 2016-03-04.
- ^ a b c Redberg, Rita F., and Smith-Bindman, Rebecca. «We Are Giving Ourselves Cancer» Archived 2017-07-06 at the Wayback Machine, New York Times, January 30, 2014
- ^ Health, Center for Devices and Radiological. «Medical X-ray Imaging – What are the Radiation Risks from CT?». www.fda.gov. Archived from the original on 5 November 2013. Retrieved 1 May 2018.
- ^ (ACR), Radiological Society of North America (RSNA) and American College of Radiology (February 2021). «Patient Safety – Radiation Dose in X-Ray and CT Exams» (PDF). acr.org. Archived from the original (PDF) on 1 January 2021. Retrieved 6 April 2021.
- ^ a b c Rehani, Madan M.; Yang, Kai; Melick, Emily R.; Heil, John; Šalát, Dušan; Sensakovic, William F.; Liu, Bob (2020). «Patients undergoing recurrent CT scans: assessing the magnitude». European Radiology. 30 (4): 1828–1836. doi:10.1007/s00330-019-06523-y. PMID 31792585. S2CID 208520824.
- ^ a b Brambilla, Marco; Vassileva, Jenia; Kuchcinska, Agnieszka; Rehani, Madan M. (2020). «Multinational data on cumulative radiation exposure of patients from recurrent radiological procedures: call for action». European Radiology. 30 (5): 2493–2501. doi:10.1007/s00330-019-06528-7. PMID 31792583. S2CID 208520544.
- ^ a b Rehani, Madan M.; Melick, Emily R.; Alvi, Raza M.; Doda Khera, Ruhani; Batool-Anwar, Salma; Neilan, Tomas G.; Bettmann, Michael (2020). «Patients undergoing recurrent CT exams: assessment of patients with non-malignant diseases, reasons for imaging and imaging appropriateness». European Radiology. 30 (4): 1839–1846. doi:10.1007/s00330-019-06551-8. PMID 31792584. S2CID 208520463.
- ^ Mathews, J. D.; Forsythe, A. V.; Brady, Z.; Butler, M. W.; Goergen, S. K.; Byrnes, G. B.; Giles, G. G.; Wallace, A. B.; Anderson, P. R.; Guiver, T. A.; McGale, P.; Cain, T. M.; Dowty, J. G.; Bickerstaffe, A. C.; Darby, S. C. (2013). «Cancer risk in 680 000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians». BMJ. 346 (may21 1): f2360. doi:10.1136/bmj.f2360. ISSN 1756-1833. PMC 3660619. PMID 23694687.
- ^ Sasieni, P D; Shelton, J; Ormiston-Smith, N; Thomson, C S; Silcocks, P B (2011). «What is the lifetime risk of developing cancer?: the effect of adjusting for multiple primaries». British Journal of Cancer. 105 (3): 460–465. doi:10.1038/bjc.2011.250. ISSN 0007-0920. PMC 3172907. PMID 21772332.
- ^ Eckel, Laurence J.; Fletcher, Joel G.; Bushberg, Jerrold T.; McCollough, Cynthia H. (2015-10-01). «Answers to Common Questions About the Use and Safety of CT Scans». Mayo Clinic Proceedings. 90 (10): 1380–1392. doi:10.1016/j.mayocp.2015.07.011. ISSN 0025-6196. PMID 26434964.
- ^ «Expert opinion: Are CT scans safe?». ScienceDaily. Retrieved 2019-03-14.
- ^ McCollough, Cynthia H.; Bushberg, Jerrold T.; Fletcher, Joel G.; Eckel, Laurence J. (2015-10-01). «Answers to Common Questions About the Use and Safety of CT Scans». Mayo Clinic Proceedings. 90 (10): 1380–1392. doi:10.1016/j.mayocp.2015.07.011. ISSN 0025-6196. PMID 26434964.
- ^ «No evidence that CT scans, X-rays cause cancer». Medical News Today. 4 February 2016. Retrieved 2019-03-14.
- ^ Kalra, Mannudeep K.; Maher, Michael M.; Rizzo, Stefania; Kanarek, David; Shephard, Jo-Anne O. (April 2004). «Radiation exposure from Chest CT: Issues and Strategies». Journal of Korean Medical Science. 19 (2): 159–166. doi:10.3346/jkms.2004.19.2.159. ISSN 1011-8934. PMC 2822293. PMID 15082885.
- ^ Rob, S.; Bryant, T.; Wilson, I.; Somani, B.K. (2017). «Ultra-low-dose, low-dose, and standard-dose CT of the kidney, ureters, and bladder: is there a difference? Results from a systematic review of the literature». Clinical Radiology. 72 (1): 11–15. doi:10.1016/j.crad.2016.10.005. PMID 27810168.
- ^ a b c d e f g h i j k l m n o p Whaites, Eric (2008-10-10). Radiography and Radiology for Dental Care Professionals E-Book. Elsevier Health Sciences. p. 25. ISBN 978-0-7020-4799-2.
- ^ a b c d e Davies, H. E.; Wathen, C. G.; Gleeson, F. V. (25 February 2011). «The risks of radiation exposure related to diagnostic imaging and how to minimise them». BMJ. 342 (feb25 1): d947. doi:10.1136/bmj.d947. PMID 21355025. S2CID 206894472.
- ^ Baysson H, Etard C, Brisse HJ, Bernier MO (January 2012). «[Diagnostic radiation exposure in children and cancer risk: current knowledge and perspectives]». Archives de Pédiatrie. 19 (1): 64–73. doi:10.1016/j.arcped.2011.10.023. PMID 22130615.
- ^ a b c d Semelka RC, Armao DM, Elias J, Huda W (May 2007). «Imaging strategies to reduce the risk of radiation in CT studies, including selective substitution with MRI». J Magn Reson Imaging. 25 (5): 900–9. doi:10.1002/jmri.20895. PMID 17457809. S2CID 5788891.
- ^ Larson DB, Rader SB, Forman HP, Fenton LZ (August 2007). «Informing parents about CT radiation exposure in children: it’s OK to tell them». Am J Roentgenol. 189 (2): 271–5. doi:10.2214/AJR.07.2248. PMID 17646450. S2CID 25020619.
- ^ a b Namasivayam S, Kalra MK, Torres WE, Small WC (Jul 2006). «Adverse reactions to intravenous iodinated contrast media: a primer for radiologists». Emergency Radiology. 12 (5): 210–5. doi:10.1007/s10140-006-0488-6. PMID 16688432. S2CID 28223134.
- ^ a b c Christiansen C (2005-04-15). «X-ray contrast media – an overview». Toxicology. 209 (2): 185–7. doi:10.1016/j.tox.2004.12.020. PMID 15767033.
- ^ a b Wang H, Wang HS, Liu ZP (October 2011). «Agents that induce pseudo-allergic reaction». Drug Discov Ther. 5 (5): 211–9. doi:10.5582/ddt.2011.v5.5.211. PMID 22466368. S2CID 19001357.
- ^ Drain KL, Volcheck GW (2001). «Preventing and managing drug-induced anaphylaxis». Drug Safety. 24 (11): 843–53. doi:10.2165/00002018-200124110-00005. PMID 11665871. S2CID 24840296.
- ^ Castells, Mariana C., ed. (2010-12-09). Anaphylaxis and hypersensitivity reactions. New York: Humana Press. p. 187. ISBN 978-1-60327-950-5.
- ^ a b c Hasebroock KM, Serkova NJ (April 2009). «Toxicity of MRI and CT contrast agents». Expert Opinion on Drug Metabolism & Toxicology. 5 (4): 403–16. doi:10.1517/17425250902873796. PMID 19368492. S2CID 72557671.
- ^ Rawson, James V.; Pelletier, Allen L. (2013-09-01). «When to Order Contrast-Enhanced CT». American Family Physician. 88 (5): 312–316. ISSN 0002-838X. PMID 24010394.
- ^ Thomsen, Henrik S.; Muller, Robert N.; Mattrey, Robert F. (2012-12-06). Trends in Contrast Media. Springer Science & Business Media. ISBN 978-3-642-59814-2.
- ^ Davenport, Matthew (2020). «Use of Intravenous Iodinated Contrast Media in Patients with Kidney Disease: Consensus Statements from the American College of Radiology and the National Kidney Foundation». Radiology. 294 (3): 660–668. doi:10.1148/radiol.2019192094. PMID 31961246.
- ^ a b c Cuttler JM, Pollycove M (2009). «Nuclear energy and health: and the benefits of low-dose radiation hormesis». Dose-Response. 7 (1): 52–89. doi:10.2203/dose-response.08-024.Cuttler. PMC 2664640. PMID 19343116.
- ^ a b «What are the Radiation Risks from CT?». Food and Drug Administration. 2009. Archived from the original on 2013-11-05.
- ^ a b c d e f Hall EJ, Brenner DJ (May 2008). «Cancer risks from diagnostic radiology». The British Journal of Radiology. 81 (965): 362–78. doi:10.1259/bjr/01948454. PMID 18440940. S2CID 23348032.
- ^ a b c d e Shrimpton, P.C; Miller, H.C; Lewis, M.A; Dunn, M. Doses from Computed Tomography (CT) examinations in the UK – 2003 Review Archived 2011-09-22 at the Wayback Machine
- ^ Michael T. Ryan; Poston, John W., eds. (2005). A half century of health physics. Baltimore, Md.: Lippincott Williams & Wilkins. p. 164. ISBN 978-0-7817-6934-1.
- ^ Polo SE, Jackson SP (March 2011). «Dynamics of DNA damage response proteins at DNA breaks: a focus on protein modifications». Genes Dev. 25 (5): 409–33. doi:10.1101/gad.2021311. PMC 3049283. PMID 21363960.
- ^ The Measurement, Reporting, and Management of Radiation Dose in CT Archived 2017-06-23 at the Wayback Machine «It is a single dose parameter that reflects the risk of a nonuniform exposure in terms of an equivalent whole-body exposure.»
- ^ Hill B, Venning AJ, Baldock C (2005). «A preliminary study of the novel application of normoxic polymer gel dosimeters for the measurement of CTDI on diagnostic X-ray CT scanners». Medical Physics. 32 (6): 1589–1597. Bibcode:2005MedPh..32.1589H. doi:10.1118/1.1925181. PMID 16013718.
- ^ Issa, Ziad F.; Miller, John M.; Zipes, Douglas P. (2019-01-01). «Complications of Catheter Ablation of Cardiac Arrhythmias». Clinical Arrhythmology and Electrophysiology. Elsevier. pp. 1042–1067. doi:10.1016/b978-0-323-52356-1.00032-3. ISBN 978-0-323-52356-1.
- ^ «Absorbed, Equivalent, and Effective Dose – ICRPaedia». icrpaedia.org. Retrieved 2021-03-21.
- ^ Materials, National Research Council (US) Committee on Evaluation of EPA Guidelines for Exposure to Naturally Occurring Radioactive (1999). Radiation Quantities and Units, Definitions, Acronyms. National Academies Press (US).
- ^ Pua, Bradley B.; Covey, Anne M.; Madoff, David C. (2018-12-03). Interventional Radiology: Fundamentals of Clinical Practice. Oxford University Press. ISBN 978-0-19-027624-9.
- ^ Paragraph 55 in: «The 2007 Recommendations of the International Commission on Radiological Protection». International Commission on Radiological Protection. Archived from the original on 2012-11-16. Ann. ICRP 37 (2-4)
- ^ «Do CT scans cause cancer?». Harvard Medical School. March 2013. Archived from the original on 2017-12-09. Retrieved 2017-12-09.
- ^ CDC (2020-06-05). «Radiation and pregnancy: A fact sheet for clinicians». Centers for Disease Control and Prevention. Retrieved 2021-03-21.
- ^ Yoon, Ilsup; Slesinger, Todd L. (2021), «Radiation Exposure In Pregnancy», StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 31869154, retrieved 2021-03-21
- ^ Wintermark M, Lev MH (January 2010). «FDA investigates the safety of brain perfusion CT». AJNR Am J Neuroradiol. 31 (1): 2–3. doi:10.3174/ajnr.A1967. PMC 7964089. PMID 19892810.
- ^ Jun, Kyungtaek; Yoon, Seokhwan (2017). «Alignment Solution for CT Image Reconstruction using Fixed Point and Virtual Rotation Axis». Scientific Reports. 7: 41218. arXiv:1605.04833. Bibcode:2017NatSR…741218J. doi:10.1038/srep41218. ISSN 2045-2322. PMC 5264594. PMID 28120881.
- ^ «Computed Tomography (CT)». www.nibib.nih.gov. Retrieved 2021-03-20.
- ^ Aichinger, Horst; Dierker, Joachim; Joite-Barfuß, Sigrid; Säbel, Manfred (2011-10-25). Radiation Exposure and Image Quality in X-Ray Diagnostic Radiology: Physical Principles and Clinical Applications. Springer Science & Business Media. p. 5. ISBN 978-3-642-11241-6.
- ^ Erdoğan, Hakan (1999). Statistical Image Reconstruction Algorithms Using Paraboloidal Surrogates for PET Transmission Scans. University of Michigan. ISBN 978-0-599-63374-2.
- ^ Themes, U. F. O. (2018-10-07). «CT Image Reconstruction Basics». Radiology Key. Retrieved 2021-03-20.
- ^ a b Stirrup, James (2020-01-02). Cardiovascular Computed Tomography. Oxford University Press. ISBN 978-0-19-880927-2.
- ^ «computed tomography – Definition from the Merriam-Webster Online Dictionary». Archived from the original on 19 September 2011. Retrieved 18 August 2009.
- ^ Webb, W. Richard; Brant, William E.; Major, Nancy M. (2014). Fundamentals of Body CT. Elsevier Health Sciences. p. 152. ISBN 978-0-323-26358-0.
- ^ Webb, Wayne Richard; Brant, William E.; Major, Nancy M. (2006-01-01). Fundamentals of Body CT. Elsevier Health Sciences. p. 168. ISBN 978-1-4160-0030-3.
- ^ Thomas, Adrian M. K.; Banerjee, Arpan K.; Busch, Uwe (2005-12-05). Classic Papers in Modern Diagnostic Radiology. Springer Science & Business Media. ISBN 978-3-540-26988-5.
- ^ Radon J (1 December 1986). «On the determination of functions from their integral values along certain manifolds». IEEE Transactions on Medical Imaging. 5 (4): 170–176. doi:10.1109/TMI.1986.4307775. PMID 18244009. S2CID 26553287.
- ^ Oldendorf WH (1978). «The quest for an image of brain: a brief historical and technical review of brain imaging techniques». Neurology. 28 (6): 517–33. doi:10.1212/wnl.28.6.517. PMID 306588. S2CID 42007208.
- ^ Richmond, Caroline (2004). «Obituary – Sir Godfrey Hounsfield». BMJ. 329 (7467): 687. doi:10.1136/bmj.329.7467.687. PMC 517662.
- ^ Frank Natterer (2001). The Mathematics of Computerized Tomography (Classics in Applied Mathematics). Society for Industrial and Applied Mathematics. p. 8. ISBN 978-0-89871-493-7.
- ^ Sperry, Len (2015-12-14). Mental Health and Mental Disorders: An Encyclopedia of Conditions, Treatments, and Well-Being [3 volumes]: An Encyclopedia of Conditions, Treatments, and Well-Being. ABC-CLIO. p. 259. ISBN 978-1-4408-0383-3.
- ^ Hounsfield, G. N. (1977). «The E.M.I. Scanner». Proceedings of the Royal Society of London. Series B, Biological Sciences. 195 (1119): 281–289. Bibcode:1977RSPSB.195..281H. doi:10.1098/rspb.1977.0008. ISSN 0080-4649. JSTOR 77187. PMID 13396. S2CID 34734270.
- ^ Miñano, Glenn (3 November 2015). «What’s the difference between a CAT-Scan and a CT-Scan? — Cincinnati Children’s Blog». blog.cincinnatichildrens.org. Retrieved 2021-03-19.
- ^ «Difference Between CT Scan and CAT Scan | Difference Between». Retrieved 2021-03-19.
- ^ Conquer Your Headaches. International Headache Management. 1994. p. 115. ISBN 978-0-9636292-5-8.
- ^ «MeSH Browser». meshb.nlm.nih.gov.
- ^ Edholm, Paul; Gabor, Herman (December 1987). «Linograms in Image Reconstruction from Projections». IEEE Transactions on Medical Imaging. MI-6 (4): 301–7. doi:10.1109/tmi.1987.4307847. PMID 18244038. S2CID 20832295.
- ^ «Image Gently». The Alliance for Radiation Safety in Pediatric Imaging. Archived from the original on 9 June 2013. Retrieved 19 July 2013.
- ^ «Image Wisely». Joint Task Force on Adult Radiation Protection. Archived from the original on 21 July 2013. Retrieved 19 July 2013.
- ^ «Optimal levels of radiation for patients». World Health Organization. Archived from the original on 25 May 2013. Retrieved 19 July 2013.
- ^ «Global Initiative on Radiation Safety in Healthcare Settings» (PDF). World Health Organization. Archived (PDF) from the original on 29 October 2013. Retrieved 19 July 2013.
- ^ «Computed tomography (CT) scanners». OECD.
- ^ Fred A. Mettler Jr; Mythreyi Bhargavan; Keith Faulkner; Debbie B. Gilley; Joel E. Gray; Geoffrey S. Ibbott; Jill A. Lipoti; Mahadevappa Mahesh; John L. McCrohan; Michael G. Stabin; Bruce R. Thomadsen; Terry T. Yoshizumi (2009). «Radiologic and Nuclear Medicine Studies in the United States and Worldwide: Frequency, Radiation Dose, and Comparison with Other Radiation Sources — 1950-2007». Radiology. 253 (2): 520–531. doi:10.1148/radiol.2532082010. PMID 19789227.
- ^ Andrew Skelly (Aug 3, 2010). «CT ordering all over the map». The Medical Post.
- ^ Korley FK, Pham JC, Kirsch TD (October 2010). «Use of advanced radiology during visits to US emergency departments for injury-related conditions, 1998–2007». JAMA. 304 (13): 1465–71. doi:10.1001/jama.2010.1408. PMID 20924012.
- ^ «Global Computed Tomography (CT) Scanners Devices and Equipment Market Report 2020: Major Players are GE Healthcare, Koninklijke Philips, Hitachi, Siemens and Canon Medical Systems – ResearchAndMarkets.com». Business Wire. November 7, 2019.
- ^ Jenkins, Ron; Gould, R W; Gedcke, Dale (1995). «Instrumentation». Quantitative x-ray spectrometry (2nd ed.). New York: Dekker. p. 90. ISBN 978-0-8247-9554-2.
- ^ Shikhaliev, Polad M.; Xu, Tong; Molloi, Sabee (2005). «Photon counting computed tomography: Concept and initial results». Medical Physics. 32 (2): 427–36. Bibcode:2005MedPh..32..427S. doi:10.1118/1.1854779. PMID 15789589.
- ^ Taguchi, Katsuyuki; Iwanczyk, Jan S. (2013). «Vision 20/20: Single photon counting x-ray detectors in medical imaging». Medical Physics. 40 (10): 100901. Bibcode:2013MedPh..40j0901T. doi:10.1118/1.4820371. PMC 3786515. PMID 24089889.
- ^ «NIH uses photon-counting CT scanner in patients for the first time». National Institutes of Health. 24 February 2016. Archived from the original on 18 August 2016. Retrieved 28 July 2016.
- ^ «Photon-counting breast CT measures up». medicalphysicsweb. Archived from the original on 2016-07-27. Retrieved 28 July 2016.
- ^ Kachelrieß, Marc; Rehani, Madan M. (March 1, 2020). «Is it possible to kill the radiation risk issue in computed tomography?». Physica Medica: European Journal of Medical Physics. 71: 176–177. doi:10.1016/j.ejmp.2020.02.017. PMID 32163886. S2CID 212692606 – via www.physicamedica.com.
External links[edit]
- Development of CT imaging
- CT Artefacts—PPT by David Platten
- Filler, Aaron (2009-06-30). «The History, Development and Impact of Computed Imaging in Neurological Diagnosis and Neurosurgery: CT, MRI, and DTI». Nature Precedings: 1. doi:10.1038/npre.2009.3267.3. ISSN 1756-0357.
- Boone, John M.; McCollough, Cynthia H. (2021). «Computed tomography turns 50». Physics Today. 74 (9): 34–40. Bibcode:2021PhT….74i..34B. doi:10.1063/PT.3.4834. ISSN 0031-9228. S2CID 239718717.
Компьютерная томография
Что это? Компьютерная томография (сокращенно КТ) – это метод диагностики, позволяющий получить точную и объективную информацию о состоянии тканей и органов, а также сосудистой системы пациента. Компьютерная томография используется для выявления новообразований, патологических процессов в органах, костных и мягких тканях, сосудах, нарушений нормального функционирования структур и систем организма. Исследование не требует специальной подготовки, за исключением исследований, проводимых с использованием рентгеноконтрастных веществ. Исследования с помощью компьютерной томографии позволяют получить более информативный результат. При этом подготовка пациента осуществляется непосредственно перед исследованием под контролем врача.
Как проводят компьютерную томографию (КТ)
При проведении компьютерной томографии пациент помещается в зону рентгеновского излучения низкой интенсивности. Процедура проводится в открытом пространстве и не вызывает дискомфорта. Длительность процедуры незначительна, так как оборудование, которое мы используем, система последнего поколения SOMATOM Perspective фирмы Siemens, существенно сокращает время исследования и лучевую нагрузку на организм пациента. Если исследование проводится с применением рентгеноконтрастного вещества, непосредственно перед исследованием пациенту вводится препарат внутривенно. Препарат безопасен и выводится из организма естественным путем в течение нескольких часов.
Кому показана компьютерная томография?
Если пациент испытывает симптомы, позволяющие предположить наличие заболевания или патологии в тканях, органах или сосудах, компьютерная томография показана, как наиболее точный и информативный метод исследования. Компьютерная томография позволит выявить проблему, локализовать ее, поставить точный диагноз и выбрать наиболее эффективное лечение. Его преимуществом является возможность тонкой диагностики в большом количестве проекций и точной локализации проблемной зоны.
Безопасен ли метод КТ?
Компьютерная томография не может быть отнесена к абсолютно безопасным исследованиям. Несмотря на то, что доза рентгеновского облучения незначительна по сравнению с рентгеновским исследованием, некоторая доза облучения в процессе исследования присутствует. В современных условиях и с применением прогрессивного медицинского оборудования риски минимизированы. Взвесив риски облучения, наши пациенты выбирают современную диагностику для предупреждения заболеваний и выявления их на самых ранних стадиях.
Записаться на прием
Оставьте нам свои контакты, и мы обязательно Вам перезвоним.
Бурлаченко Евгений
Петрович
Заведующий отделением лучевой диагностики. Врач КТ
Стаж работы : c 1989 года
Подробнее
Компьютерная томография (КТ) – это метод диагностики, основанный на послойном исследовании структуры внутренних органов и систем; данные получаются с помощью рентгенологического оборудования, совмещенного с мощной компьютерной станцией, позволяющей проводить оперативный детальный анализ изображения.
Как устроен томограф
Компьютерная томография
Главная часть любого современного томографа это гентри – кольцо, внутри которого быстро вращается лучевая трубка, напротив которой расположены датчики. Пациент ложится на двигающийся стол, перемещающийся внутри этого кольца. Движение стола и рентгеновской трубки синхронизированы так, чтобы в результате считывание информации осуществлялось по спирали, обходящей тело пациента в области отдела, подлежащего исследованию, со всех сторон. Подобное исследование еще называется мультиспиральной компьютерной томогорафией (МСКТ). Приставка «мульти» означает, что в современных томографах датчики установлены не в один ряд (таких рядов может быть много). Это позволяет не только получать больше информации за один оборот лучевой трубки (что увеличивает скорость обследования и снижает лучевую нагрузку), но и отследить работу динамических органов и структур (сердца, грудной клетки, суставов в движении).
Преимущества компьютерной томографии (МСКТ) как метода диагностики
Компьютерная томография является одним из лучших неинвазивных (осуществляемых без повреждения тканей) диагностических методов. Высокая разрешающая способность МСКТ в сочетании с передовым программным обеспечением, позволяющим реконструировать очень тонкие срезы, визуализируют изменения, размеры которых не превышают даже нескольких миллиметров, что дает возможность обнаруживать заболевания на самых ранних стадиях.
В некоторых случаях проводится компьютерная томография с болюсным контрастированием. Современные томографы оборудованы встроенным автоматическим инъектором, с помощью которого через специальный катетер в локтевую вену вводится контрастное вещество. Работа инъектора синхронизирована с процессом сканирования. Болюсное контрастирование позволяет оценить характер накопления контрастного вещества, что расширяет возможности диагностики. В качестве контрастного вещества при болюсном контрастировании используются йодсодержащие препараты.
Важными преимуществами компьютерной томографии также являются:
- возможность получения объемных изображений внутренних органов;
- быстрота проведения (само исследование длится менее полминуты, дольше одеваться);
- комфорт (пациент не испытывает неприятных ощущений).
Что исследуется с помощью МСКТ (мультиспиральной компьютерной томографии)?
Компьютерные реконструкции
Мультиспиральная компьютерная томография используется для исследования следующих органов и областей организма:
- головной мозг. МСКТ головного мозга позволяет выявлять различные заболевания серого и белого вещества мозга, а также нарушения со стороны окружающих тканей, оболочек и сосудов. Могут быть выявлены аномалии развития, воспалительные очаги, доброкачественные и злокачественные новообразования, сосудистые расстройства, кровоизлияния, гематомы, геморрагические и ишемические инсульты;
- кости черепа. Востребованными исследованиями являются МСКТ лицевого отдела черепа и МСКТ височных костей, которая проводится с высокой детализацией костной ткани;
- носовые пазухи. Реконструкция в двух и более проекциях дает возможность обнаружить причины заложенности носа и снижения обоняния, определить наличие гноя в пазухах, выявить полипы и дефекты носовых ходов. В рамках одного исследования может проводиться МСКТ пазух носа и височных костей.
- органы грудной клетки. МСКТ органов грудной клетки позволяет исследовать легкие, плевру, трахею и бронхи, органы средостения: пищевод, сердце, аорту, лимфатические узлы, молочные железы. С помощью МСКТ могут быть выявлены туберкулез, пневмония, доброкачественные и раковые опухоли различной локализации, аномалии развития, посттравматические изменения, сосудистые нарушения и другие заболевания;
- позвоночник. МСКТ позвоночника – более информативное исследование, чем обычная рентгенография. Оно позволяет получить объемную картину, увидеть позвоночник в различных проекциях, что расширяет возможности диагностики состояния межпозвоночных дисков, повреждений тел позвонков и отростков, состояния позвоночного столба.
- органы брюшной полости и забрюшинного пространства. МСКТ брюшной полости и забрюшинного пространства позволяет визуализировать мягкие ткани этой области. Исследуются печень, желчный пузырь, желчевыводящие пути, поджелудочная железа, селезенка, толстый и тонкий кишечник, почки, надпочечники, мочеточники, а также лимфоузлы и сосуды. Исследование позволяет оценить размер и положение органа, обнаружить патологические образования и диффузные изменения (очаг воспаления, абсцесс и т.п.). Если локализация проблем известна, проводится МСКТ конкретного органа – печени, желчного пузыря и поджелудочной железы; почек и надпочечников; или только надпочечников;
- кишечник. МСКТ позволяет проводить исследование кишечника с созданием объемной (3D) реконструкции изображения органа;
- органы малого таза. При МСКТ органов малого таза обследуются тазовые кости, мочевой пузырь, у женщин — матка и яичники, у мужчин — предстательная железа и семенные пузырьки;
- суставы. МСКТ суставов позволяет обнаружить патологические процессы, происходящие в костях и мягких тканях, составляющих сустав. Чаще всего исследуются тазобедренный и коленный суставы;
- сосуды. МСКТ дает возможность оценить состояние сосудов диаметром от 1 мм. Обследуются сосуды различных областей — головного мозга, шеи, нижних конечностей, аорта и подвздошные артерии;
- глазные орбиты. МСКТ глазных орбит позволяет выявить структурные нарушения глазного яблока, костной основы глазницы, глазодвигательных мышц, глазного нерва, слезных желез.
Компьютерная томография в «Семейном докторе»
В «Семейном докторе» используются томографы нового поколения GE OPTIMA CT660 производства GE Healthcare (подразделение корпорации General Electric, США). Данный аппарат делает 64 изображения-среза за один оборот, что значительно ускоряет процесс диагностики. Отличительной особенностью аппарата является его высокая разрешающая способность, позволяющая создавать качественную двухмерную (2D) и трехмерную (3D) реконструкцию изображений.
Другие преимущества GE OPTIMA CT660:
- улучшенная эргономика сканера, обеспечивающая пациенту максимальный комфорт;
- настройка параметров сканирования осуществляется в присутствии пациента, таки образом у него есть время, чтобы освоиться;
- диагностика проводится буквально за секунды, при этом доза облучения оптимизируется, чтобы обеспечить минимально возможную лучевую нагрузку.
МСКТ-исследование
Поликлиники, в которых оказываются услуги компьютерной томографии, можно посмотреть по ссылке>>>
Что нужно знать, направляясь на компьютерную томографию
Чтобы пройти МСКТ, необходимо направление от врача, в котором бы указывались область и цель исследования. При направлении на МСКТ с болюсным контрастированием также необходимо иметь на руках заключение аллерголога с разрешением на проведение исследования или рекомендациями о предварительной подготовке. Если у Вас на руках нет направления, Вы можете обратиться в любую из поликлиник «Семейного доктора», записавшись на прием к врачу-специалисту или врачу общей практики. Вас осмотрит опытный специалист, даст свои рекомендации и выпишет направление на МСКТ.
В зависимости от области исследования, Вам может потребоваться подготовка к прохождению МСКТ. Например, МСКТ печени и желчного пузыря делаются утром строго натощак. МСКТ почек или органов малого таза можно делать в течение дня, при этом допустим легкий завтрак. МСКТ головного мозга, носовых пазух, органов грудной клетки, костей и суставов можно делать в любое время, так как специальной подготовки к данным исследованиям не требуется.
Для более точного, индивидуального подбора программы проведения МСКТ и прицельной реконструкции изображений желательно иметь при себе все медицинские документы, отражающие историю заболевания. Возьмите с собой все имеющиеся у Вас результаты прошлых исследований (рентген, УЗИ, УЗЛГ, КТ, МРТ, ПЭТ). Весь ваш архив будет вам полностью возвращен вместе с результатами МСКТ.
Во время прохождения исследования Вам потребуется по указанию врача сохранять неподвижное положение и задержать дыхание на 10-20 секунд.
Есть вопросы?
Оставьте телефон –
и мы Вам перезвоним
Записаться на диагностику
Не занимайтесь самолечением. Обратитесь к нашим специалистам, которые правильно поставят диагноз и назначат лечение.
Фото и видео галерея
ЧТО ТАКОЕ КОМПЬЮТЕРНАЯ ТОМОГРАФИЯ?
Еще в середине прошлого века для исследования внутренней структуры тела начали применяться специальные сканеры – компьютерные томографы, которые управлялись ламповыми ЭВМ. Но даже такие машины могли получать изображение какого-либо среза тела, разумеется, в гораздо худшем качестве по сравнению с современными машинами. Компьютерная томография – это способ получить «срез» тела человека, не причиняя ему существенного физического воздействия. Еще основоположник топографической анатомии – Пирогов Н. И. – изготовлял срезы замороженных человеческих тел с научной и образовательной целью, но для прижизненной диагностики болезней такой способ не был пригоден.
Основной инструмент для проведения КТ – томограф. Он состоит из следующих основных частей: кольцо (гентри), в которое вмонтирована рентгеновская трубка или несколько трубок, движущаяся по кругу вокруг стола и пациента; стол, который может перемещаться вместе с пациентом внутри гентри; компьютер, который преобразует полученные данные в вид, удобный для анализа человеком, и выводит полученные изображения на экран. Формат изображений, используемый в медицинских целях, называется dicom (от англ. «digital images and communications in medicine» – «цифровые изображения медицинского назначения и способы их передачи»). Данные в этом формате можно просмотреть, используя специальные программы – «просмотрщики».
Сделать КТ в Санкт-Петербурге
Принцип работы компьютерного томографа состоит в следующем: рентгеновская трубка совершает обороты вокруг исследуемого объекта и испускает рентгеновское излучение определенной энергии. Рентгеновское излучение проникает через тело насквозь и достигает противоположной части кольца, где находятся приемные устройства (детекторы). Под различным углом коэффициент ослабления рентгеновских лучей различен, т. к. они проходят через разный массив тканей (по толщине и по плотности). В результате детекторы воспринимают определенную информацию (угол, под которым был послан рентгеновский электромагнитный сигнал и его энергию). В итоге по окончанию сканирования вся информация собирается и анализируется центральным процессором томографа, а затем преобразуется в удобный для восприятия человеком вид – в изображения. В последующем анализ этих изображений осуществляется врачом-рентгенологом.
Так выглядит компьютерный томограф (1 — гентри, 2 – панель управления, 3 – стол).На изображении – 16-срезовый аппарат фирмы General Electrics Healthcare из серии BrightStar Elite.
ЗАЧЕМ ДЕЛАТЬ КТ? КТО НАЗНАЧАЕТ КТ?
Существует множество показаний для компьютерной томографии. В целом все исследования можно разделить на несколько групп в зависимости от экстренности и тяжести случая. К первой группе можно отнести исследования, выполняемые по экстренным показаниями больным с травмой различной локализации (черепно-мозговой, травмой живота, грудной клетки, конечностей); больным с нарушением кровообращения в мозге (ишемический и геморрагический инсульты, субарахноидальные кровоизлияния). Так как КТ выполняется быстро (несколько минут), и полученные при КТ данные имеют высокую информативность, КТ предпочтительнее МРТ при данной патологии.
Ко второй группе можно отнести исследования пациентов с уже выявленной посредством других методов (УЗИ, МРТ, рентгенография) патологией. Так, например, КТ органов живота показано пациенту с выявленным раком кишечника (например, посредством ректороманоскопии) с целью уточнить, имеются ли отдаленные метастазы в органы и лимфатические узлы. Если метастазов не выявлено, а опухоль обладает экспансивным ростом, не прорастает в окружающие ткани, возможно оперативное лечение. Выявление отдаленных метастазов в большей части случаев делает операцию нецелесообразной.
И, наконец, к третьей группе относятся исследования, выполняемые с целью исключить либо подтвердить патологию, обнаруженную «классическими» методами диагностики. Так, обнаружение симптомов панкреатита в совокупности с изменениями в биохимическом анализе крови (повышением уровня амилазы) позволяют предположить острый панкреатит. При КТ оценивается степень выраженности отека панкреатической клетчатки, локализация воспалительного процесса (головка, тело либо панкреатический хвост), наличие свободной жидкости в брюшной и грудной полостях.
К четвертой группе относятся профилактические, скрининговые исследования. В РФ они мало распространены в связи с малой доступностью компьютерной томографии, в то же время в странах Европы стандартную флюорографию все больше заменяет КТ-исследование грудной клетки с малой дозой облучения. Эффективность таких исследований выше при сравнимой лучевой нагрузке.
Компьютерную томографию может назначить врач при выявлении у пациента характерных жалоб для исключения или подтверждения заболевания (например, воспалительных заболеваний легких, органов брюшной полости и т. д.). Сейчас можно пройти КТ и без врачебного направления – по собственному желанию – в многочисленных частных платных центрах. Однако нужно учитывать, что пациент не всегда адекватно может оценить степень необходимости конкретного исследования, поэтому, чтобы не тратить впустую свои деньги и не получать дозу облучения, целесообразно проконсультироваться с врачом о необходимости процедуры.
КАКИЕ БЫВАЮТ ВИДЫ КТ?
В первую очередь все КТ-исследования можно разделить по областям тела. Так, чаще всего выделяют КТ:
- КТ головного мозга и черепа
- КТ придаточных околоносовых пазух
- КТ челюстей и зубов (дентальная КТ)
- КТ височных костей
- КТ мягких тканей шеи
- КТ кранио-вертебральной области
- КТ шейного отдела позвоночного столба
- КТ грудной клетки
- КТ грудного отдела позвоночника
- КТ органов брюшной полости и забрюшинного пространства
- КТ поясничного отдела позвоночника
- КТ малого таза
- КТ тазобедренных суставов
- КТ коленных суставов
- КТ верхних или нижних конечностей.
КТ-исследования можно выполнять без контрастного усиления и с контрастным усилением. В первом случае сканируется определенная часть тела «как есть». Контрастирование также может выполняться по-разному. Контрастное вещество можно ввести в вену – это внутривенное контрастирование, можно ввести в желудок, приняв через рот взвесь сульфата бария либо жидкое контрастное средство, например, раствор урографина. КТ-фистулография подразумевает сканирование участка тела после введения контраста в свищ с целью оценить его ход, протяженность, наличие затеков.
Для внутривенного контрастирования используются ионные и неионные контрасты, содержащие йод. Ионные контрастные средства (урографин) – наиболее старые, обладающие большим количеством побочных действий. Йод в таких средствах находится в ионной форме, что и обуславливает его большую токсичность. Неионные средства (ультравист, омнипак, йодгексол, йопромид) содержат связанный йод, что повышает их безопасность при использовании.
Сульфат бария в виде взвеси – так же, как и при обычных рентгеновских исследованиях – используется для контрастирования органов системы пищеварения. Однако более целесообразным считается использование водных растворов обозначенных выше средств. Для фистулографии можно использовать урографин либо любое другое ионное (неионное) средство. Кроме того, желудок можно законтрастировать обычной водой.
ЧТО ПРОИСХОДИТ ВО ВРЕМЯ КТ?
Как делается КТ-исследование? Если исследование выполняется без контраста, не требуется никакой специальной подготовки в большинстве случаев. Пациент проходит в помещение, где установлен томограф, снимает верхнюю одежду и обувь, а также все металлические предметы (они могут стать причиной артефактов на диагностических изображениях и затруднить визуализацию патологии). Затем, следуя указаниям персонала, пациент ложится на стол головой либо ногами к гентри – на спину, на живот или на бок. Если это необходимо, рентгенлаборант фиксирует пациента к столу. При проведении сканирования от пациента может потребоваться задержать дыхание на непродолжительное время (при исследовании грудной клетки и живота) либо (при исследовании гортани и голосовых складок) произносить протяжные звуки (томография гортани с фонацией).
Сколько длится КТ-исследование? Сканирование человеческого тела занимает несколько секунд. Продолжительность сканирования зависит от величины исследуемого органа. Например, исследование околоносовых пазух длится не более 2-3 секунд, сканирование всей грудной клетки и живота — 10-15 секунд. В случае, если КТ делается с контрастированием, сканирование может повторяться несколько раз.
При КТ с контрастом в вену вводится катетер с широким просветом. Такие катетеры используются с целью максимально снизить давление контраста на стенку вены и не допустить ее повреждение. Катетер при помощи гибкого тонкого шланга соединяется с инжектором, автоматически подающим контраст с определенной скоростью. В зависимости от состояния вены скорость введения может варьировать от 1,0 до 5,0 мл/сек.
Какие ощущения бывают при КТ? Само по себе воздействие рентгеновских лучей на организм человека не вызывает совершенно никаких ощущений. При введении контрастного вещества может появиться ощущение тепла, распространяющегося по телу, учащение дыхания, сердцебиения. Это нормальные явления, они обычно проходят после окончания процедуры.
КАК ПОДГОТОВИТЬСЯ К КОМПЬЮТЕРНОЙ ТОМОГРАФИИ?
К исследованиям головы, легких и конечностей готовиться не надо. При исследовании органов брюшной полости необходимо за сутки ограничить прием трудной для усвоения пищи, на исследование прийти голодным (с пустым желудком). Если показано внутривенное контрастирование, подготовка более тщательная: она включает в себя биохимический анализ крови с целью определения показателей выделительной функции почек (креатинин, мочевина), а также сахара. Обязательно выясняется переносимость йода – с этой целью проводится простая проба – внутрикожно вводится 0,5-1,0 мл планируемого для использования контраста. Если через 10-15 минут нет никаких проявлений аллергии в виде покраснения кожи, зуда и возникновения пузырьков, контраст вводить можно.
Важно: собираясь на КТ, захватите с собой все результаты предыдущих исследований, имеющих отношение к заболеванию – это могут быть рентгеновские снимки, диски с записью КТ- и МР-исследований, карта амбулаторного пациента. Возьмите также пеленку или полотенце, бахилы или сменную обувь.
КАКОВА ЛУЧЕВАЯ НАГРУЗКА ПРИ КТ?
Насколько вредно делать КТ? Компьютерная томография – это рентгеновский метод исследования, связанный с облучением тела человека. Поэтому, даже несмотря на прогресс в аппаратуре, делать это исследование небезвредно. При этом нужно понимать, что доза, полученная при компьютерной томографии, не превышает значения, которые не причиняют доказанного вреда здоровью.
В зависимости от области сканирования, от массы и объема облученных тканей, полученная доза может варьировать в значительной степени – от 0,1 до 50 мЗв.
Основополагающие моменты, от которых зависит доза:
— зона сканирования – при облучении конечностей доза меньше, чем при облучении живота, таза или грудной клетки;
— протяженность зоны сканирования – чем она больше, тем выше доза;
— объем облученных тканей – чем плотнее человек, чем больше его объемы, тем более значительное биологическое воздействие оказывает на его организм КТ;
— шаг томографа или ширина витка спирали при послойном и спиральном сканировании соответственно – чем эти показатели меньше, тем больше доза;
— количество рядов детекторов в томографе – так, 16-срезовые машины более «щадящи» по сравнению с 128- и 256-срезовыми аппаратами.
В таблице рассмотрена зависимость эквивалентной дозы за одно сканирование (указаны ее минимальные и максимальные значения) от зоны исследования у «среднего» взрослого человека весом 70-75 кг, обычного телосложения. Данные приведены на основании собственных наблюдений, выборка более 5000 исследований.
| Зона сканирования | Эквивалентаная доза (мЗв) |
| Головной мозг | 1,8-3,5 |
| Придаточные пазухи носа | 0,8-2,0 |
| Височные кости | 0,8-1,5 |
| Шея: мягкие ткани, позвоночник | 2,0-5,0 |
| Грудная клетка | 5,0-12,0 |
| Органы брюшной полости | 5,0-20,0 |
| Органы малого таза | 5,0-15,0 |
| Поясничный отдел позвоночника | 5,0-15,0 |
| Грудной отдел позвоночника | 5,0-12,0 |
| Конечности | 0,1-5,0 |
Для сравнения – эквивалентная доза при цифровой флюорографии составляет примерно 0,03 мЗв (однократно).
КАК ДОЛГО ЖДАТЬ ОТВЕТА КТ?
Как долго готовятся результаты КТ? В большинстве случаев для интерпретации результатов КТ-исследования врачом-рентгенологом необходимо 30-60 минут. Кроме того, несколько десятков минут может занять распечатка пленки с изображениями, запись DICOM на диск, а также консультации с коллегами (при необходимости, в затруднительных случаях). Однако выдачи результатов можно ожидать и дольше – до суток – в случае, если исследование неординарное, либо в учреждении большой поток пациентов на одного врача. В частных центрах стремятся выдать заключение, распечатки и диск в течение 40-60 минут, в государственных учреждениях, возможно, придется ждать дольше.
КТ И ВТОРОЕ МНЕНИЕ
КТ — очень ценный метод диагностики, но иногда даже после его выполнения диагноз может оставаться неточным. Мало кто задумывается о том, что уровень и качество аппаратуры имеет хотя и важное, но не первостепенное значение. Самое главное в процессе диагностики — это правильный анализ полученных снимков. Достоверность интерпретации результатов КТ зависит, естественно, от квалификации врача: чем она выше, тем более достоверной будет диагностика. В обратном случае, даже потратив большие деньги на исследование, Вы можете оказаться без точного диагноза. Увы, в России такое происходит нередко.
Сегодня есть способ перепроверить результаты КТ, и отправить снимки на консультацию опытным специалистам, которые давно специализируются на Вашем заболевании. Если у Вас нет такого специалиста, найти его поможет Национальная телерадиологическая сеть — система дистанционных консультаций врачей-радиологов. Эта служба связывает пациентов и медицинских специалистов из крупнейших медицинских центров Москвы и Санкт-Петербурга. Достаточно зайти на сайт rentgen-online.ru, выбрать нужного врача и отправить ему КТ с диска через интернет , выполнив несколько простых действий. Через 24 часа Вы получите подробное официальное заключение с его подписью!
Василий Вишняков, врач-радиолог
Читать подробнее о Втором мнении
Читать подробнее о телемедицине
Кандидат медицинских наук, член Европейского общества радиологов
КТ (компьютерная томография) – это метод диагностики и обследования организма человека. Инструментальный тест необходимо проводить с применением специального оборудования – компьютерного томографа. Отсюда и пошло само название. По сути, КТ является современным вариантом рентгена. Благодаря КТ можно получить послойное изображение интересующего объекта (головы, коленного сустава, печени, почек и др.). В результате можно выстроить объемную картину, а не плоскую проекцию, как происходит в случае с рентгеном.
Суть метода
КТ близка к МРТ (магнитная-резонансная томографии). Однако КТ чаще всего используют с целью изучить твердые ткани (кости конечностей, черепа и т.п.), а МРТ – мягких тканей. Также, есть технические отличия этих методов, связанные с природой излучения, частотой и иными параметрами двух аппаратов, с помощью которых проводят тест.
Компьютерную томографию (КТ) относят к современным методам исследования, благодаря которым можно получить объективную картину и поставить точный диагноз. Перечислим основные достоинства данного вида диагностики:
- высокая скорость проведения (к примеру, если задержать дыхание на 15-20 секунд секунд, можно получить полную картину по органам брюшной полости);
- большая зона покрытия (позволяет одновременно исследовать несколько частей тела и органов (к примеру, грудь и живот);
- благодаря отличному пространственному разрешению получается детальная картина;
- сниженная нагрузка излучения в сравнении с рентгеновскими методами;
- безболезненность процедуры, не вызывающей никакого дискомфорта;
- риск врачебной ошибки практически исключен, поскольку получаются объективные данные.
Но есть и недостатки у такого способа диагностики:
- при частых воздействиях лучевое излучение вредно для организма;
- КТ является дорогостоящей процедурой;
- проводить компьютерную томографию во время беременности можно только по согласованию с врачом.
Содержание
- Виды компьютерной томографии
- Показания к проведению КТ
- Противопоказания и осложнения
- Показывает ли КТ онкологию
- Подготовка к КТ
- Подготовка к КТ с болюсным (контрастным) усилением
- Как проходит КТ
- Расшифровка результатов
Виды компьютерной томографии
Виды компьютерной томографии можно разделить в зависимости от того, какое назначения исследования существует:
- KТ внутренних органов (брюшная полость, почки, легких, малый таз, печень, надпочечники, брюшная аорта, грудная клетка, мочевой пузырь, желчный пузырь, поджелудочная железа, кишечник).
- KТ головы и головного мозга (головной мозг, придаточные пазухи носа, височные кости, лицевые кости, сосуды головного мозга, челюсть, глазница, гортань, зубы, мягкие ткани шеи, череп, турецкий седл, внутреннее ухо).
- KТ суставов (коленный сустав, тазобедренный сустав, плечевой сустав, локтевой сустав, стопа, кисть, голеностопный сустав, лучезапястный сустав).
- КТ позвоночника (шейный отдел, грудного отдел и пояснично-крестцовый отдел позвоночника).
- КТ сердца и сосудов (сердце, коронарные сосуды, сосуды шеи).
- Прочие KТ исследования (грудная аорта, кости таза, нижние конечности).
Рассмотрим, что определяют наиболее распространенные исследования:
- КТ головного мозга определяет патологии в головном мозге или его оболочках. Можно подразделить на несколько типов – нативная, где не вводятся контрастные вещества, усиленная (с их введением), ангиография, где вводится одна порция контрастного вещества.
- КТ височной кости позволяет уточнить причины головокружения и ухудшения слуха.
- КТ щитовидной железы используется с целью определить зоб и другие болезни.
- КТ грудной клетки позволяет получмть изображения ребер, суставов грудного отдела позвоночника, а также используют при травмах живота.
- КТ внутреннего уха является современным методом диагностики, который уточняет состояние цистерн головного мозга.
- КТ носа изучает носовую полость и пазухи.
- КТ гортани дает подробную диагностику травм и болезней гортани.
- КТ легких изучает легочную ткань, плевры, в т.ч. для диагностики поражения при COVID-19.
- КТ орбит обследует глазное яблоко, а также зрительный нерв.
Показания к проведению КТ
КТ проводят в самых различных случаях. В основном назначают для первичного и повторного обследования, а также с целью подтверждения неуточненного диагноза. Чаще всего КТ проводят при наличии:
- Мочекаменной болезни;
- Туберкулеза;
- Остеопороза;
- Болезни органов ЖКТ;
- Пневмонии;
- Онкологических патологий;
- Астмы;
- Хронического бронхита;
- Разных повреждений костей, в т.ч. позвоночника;
- Сколиоза;
- Аденомы;
- Аневризмы;
- Новообразований, которые найдены в щитовидной железе.
Бывают экстренные случаи, когда стоит проводить КТ — тяжелые травмы, подозрения кровоизлияний в мозге, повреждения крупных сосудов, паренхимы.
Противопоказания и осложнения
Бывают случаи, когда проведение компьютерной томографии противопоказано. Основными выделяют:
- беременность;
- сахарный диабет декомпенсированного типа;
- плазмоклеточная дискразия;
- почечная недостаточность;
- период лактации;
- тяжелые патологии сердца;
- миелома.
Показывает ли КТ онкологию
Компьютерная томография (КТ) способна эффективно выявить изменения, опухоль и метастазы размером от одного миллиметра в следующих органах и системах:
- головной мозг;
- кожный покров;
- органа брюшной полости и малого таза;
- кишечник
- сосуды;
- легкие и бронхи;
- позвоночник;
- мягкие ткани;
- лимфоузлы;
- кости.
Онкологи могут назначить КТ с целью уточнить диагноз, либо определить решение для дальнейшей тактики лечения.
Подготовка к КТ
За 1-2 дня до исследования необходимо исключить из рациона питания свежие овощи, фрукты, кисломолочные продукты, свежий черный хлеб, газированные напитки, бобовые культуры, крепкий кофе, алкоголь!
Перед исследованием КТ органов брюшной полости:
- За 6-8 часов ничего не есть, не пить чай, кофе.
- За 3 часа не курить.
- За 1 час выпить 3 таблетки «Нош-па», запивая стаканом простой воды (для того, чтобы убрать перистальтику кишечника).
- Если Пациент страдает запорами – за 2 часа — клизма «Микролакс».
Перед исследованием КТ забрюшинного пространства:
- За 6-8 часов ничего не есть.
- За 3 часа не курить.
- За 1 час выпить 3 таблетки «Нош-па», запивая стаканом простой воды (для того, чтобы убрать перистальтику кишечника).
- За 1 час не мочиться.
- Если Пациент страдает запорами – за 2 часа — клизма «Микролакс».
Перед исследованием КТ органов малого таза:
- За 6-8 часов ничего не есть. Не пить чай, кофе.
- За 3 часа не курить!
- За 1 час выпить 3 таблетки «Нош-па», запивая стаканом простой воды (для того, чтобы убрать перистальтику кишечника). После этого пить нельзя.
- За 1 день принимать симетикон («Боботик» / «Эспумизан» / «Симеотик») по 2 капсулы 3 раза в день.
Перед исследованием КТ ЖКТ:
- За 2-3 дня исключить из рациона: сладости, бобовые, капусту, пшеничный хлеб, молоко, сдоба и т.п. Принимать активированный уголь по 1 таблетке 2-3 раза в день.
- За 8 часов ничего не есть и не пить.
Подготовка к КТ с болюсным (контрастным) усилением
Перед проведением КТ с применением контрастного вещества нужно проконсультироваться у лечащего врача или анестезиолога. Консультация необходима в случае присутствия препаратов:
- бета-адреноблокаторов;
- интерлейкина;
- метформина;
- глюкофажа;
- гуанидинов;
- нестероидных противовоспалительных препаратов.
Помимо этого, предварительное общение со специалистами требуется тем, кто страдает следующими заболеваниями:
- Хронические почечные заболевания.
- Патологии щитовидной железы (гипертиреоз, папиллярный или фолликулярный рак щитовидной железы), а также при планировании сцинтиграфии.
- Сахарный диабет (диабетическая нефропатия).
- Бронхиальная астма, полиаллергия.
- Заболевания сердца (при сердечной недостаточности 3 или 4 степени либо недавних сердечных приступах).
- При наличии в анамнезе человека умеренных или тяжелых реакций на контрастное вещество.
Также может быть проведено дополнительное лабораторное обследование и предложены альтернативные методы диагностики (МСКТ или УЗИ).
Перед проведением компьютерной томографии с контрастным усилением необходимо отказаться от приема пищи за 4 часа до начала процедуры.
Как проходит КТ
Процедура для пациента проходит достаточно быстро и безболезненно. Исследование занимает приблизительно 15-20 минут (время зависит от обследуемой части тела). Какой-либо специальной подготовки к проведению КТ не требуется. Пациенту будет достаточно просто разуться, надеть медицинский халат и лечь на стол, автоматически задвигающийся внутрь аппарата.
После проводится несколько снимков, затем стол выкатывается обратно, пациент обувается и покидает помещение. Результаты будут сделаны через 30 минут. В некоторых случаях требуется использование контрастного вещества, которое вводят внутривенно (заранее ставят укол). В случае противопоказаний (аллергия, сахарный диабет декомпенсированный, миелома и т.д.) контраст не ставится.
При необходимости пациенту ставят седацию (легкий наркоз) с целью более комфортного прохождения процедуры. Такой метод применяют для детей и людей, которые боятся замкнутых пространств. Также седацию делают тем, кому трудно лежать в одном положении в течение нескольких минут.
Расшифровка результатов
Пациенту выдают на руки снимки или запись компьютерной томографии на электронном носителе и письменное заключение рентгенолога, в котором врач детально описывает размер, форму, положение и взаимное расположение органов, а также отмечает выявленные отклонения от нормы, в т.ч. врождённые аномалии развития. Затем врач описывает все обнаруженные образования: киста, абсцесс, камни, опухоль и т.д.
Если двигаться во время проведения и работы КТ-исследования, глубоко дышать, то это может повлиять на результаты. Искажения также могут внести металлические элементы, которые есть в организме (протез или имплантат). Об их наличии необходимо предупреждать врача заблаговременно. Если пациент принимает препараты, которые содержат висмут, то компьютерную томографию откладывают.
Достоверность расшифровки изображений КТ при диагностике рака зависит от опыта врача-рентгенолога и онколога. В частности, это важно при запутанных диагностических случаях. Медицинские ошибки могут встретиться также в описании размеров опухоли, лимфатических узлов, или других важных характерных признаков. В медицинском центре «Клиника ДНК» в Дубне работают опытные узкопрофильные специалисты, благодаря которым процент человеческих ошибок сводиться к минимуму. Компьютерная томография у нас проводится на аппарате новейшего поколения Somatom от мирового лидера компании Siemens на ежедневной основе. Быстрое и эффективное сканирование в повседневной практике позволяет выполнять сканирование с низкой лучевой нагрузкой, что очень важно для оптимальной заботы о пациенте. SOMATOM выполняет сканирование больших диапазонов за одну задержку дыхания с высоким пространственным разрешением. Записаться на КТ Вы можете онлайн или по телефону. Будьте здоровы!
Записаться на диагностику