This article is about the nature, production, and uses of the radiation. For the method of imaging, see Radiography. For the medical specialty, see Radiology. For other uses, see X-ray (disambiguation). Not to be confused with X-wave or X-band.
Natural color X-ray photogram of a wine scene. Note the edges of hollow cylinders as compared to the solid candle.
An X-ray, or, much less commonly, X-radiation, is a penetrating form of high-energy electromagnetic radiation. Most X-rays have a wavelength ranging from 10 picometers to 10 nanometers, corresponding to frequencies in the range 30 petahertz to 30 exahertz (3×1016 Hz to 3×1019 Hz) and energies in the range 145 eV to 124 keV. X-ray wavelengths are shorter than those of UV rays and typically longer than those of gamma rays. In many languages, X-radiation is referred to as Röntgen radiation, after the German scientist Wilhelm Conrad Röntgen, who discovered it on November 8, 1895.[1] He named it X-radiation to signify an unknown type of radiation.[2] Spellings of X-ray(s) in English include the variants x-ray(s), xray(s), and X ray(s).[3] The most familiar use of X-rays is checking for fractures (broken bones), but X-rays are also used in other ways. For example, chest X-rays can spot pneumonia. Mammograms use X-rays to look for breast cancer.
History[edit]
Pre-Röntgen observations and research[edit]
Before their discovery in 1895, X-rays were just a type of unidentified radiation emanating from experimental discharge tubes. They were noticed by scientists investigating cathode rays produced by such tubes, which are energetic electron beams that were first observed in 1869. Many of the early Crookes tubes (invented around 1875) undoubtedly radiated X-rays, because early researchers noticed effects that were attributable to them, as detailed below. Crookes tubes created free electrons by ionization of the residual air in the tube by a high DC voltage of anywhere between a few kilovolts and 100 kV. This voltage accelerated the electrons coming from the cathode to a high enough velocity that they created X-rays when they struck the anode or the glass wall of the tube.[4]
The earliest experimenter thought to have (unknowingly) produced X-rays was William Morgan. In 1785, he presented a paper to the Royal Society of London describing the effects of passing electrical currents through a partially evacuated glass tube, producing a glow created by X-rays.[5][6] This work was further explored by Humphry Davy and his assistant Michael Faraday.
When Stanford University physics professor Fernando Sanford created his «electric photography», he also unknowingly generated and detected X-rays. From 1886 to 1888, he had studied in the Hermann von Helmholtz laboratory in Berlin, where he became familiar with the cathode rays generated in vacuum tubes when a voltage was applied across separate electrodes, as previously studied by Heinrich Hertz and Philipp Lenard. His letter of January 6, 1893 (describing his discovery as «electric photography») to the Physical Review was duly published and an article entitled Without Lens or Light, Photographs Taken With Plate and Object in Darkness appeared in the San Francisco Examiner.[7]
Starting in 1888, Philipp Lenard conducted experiments to see whether cathode rays could pass out of the Crookes tube into the air. He built a Crookes tube with a «window» at the end made of thin aluminium, facing the cathode so the cathode rays would strike it (later called a «Lenard tube»). He found that something came through, that would expose photographic plates and cause fluorescence. He measured the penetrating power of these rays through various materials. It has been suggested that at least some of these «Lenard rays» were actually X-rays.[8]
In 1889, Ukrainian-born Ivan Puluj, a lecturer in experimental physics at the Prague Polytechnic who since 1877 had been constructing various designs of gas-filled tubes to investigate their properties, published a paper on how sealed photographic plates became dark when exposed to the emanations from the tubes.[9]
Helmholtz formulated mathematical equations for X-rays. He postulated a dispersion theory before Röntgen made his discovery and announcement. He based it on the electromagnetic theory of light.[10][full citation needed] However, he did not work with actual X-rays.
In 1894, Nikola Tesla noticed damaged film in his lab that seemed to be associated with Crookes tube experiments and began investigating this invisible, radiant energy.[11][12] After Röntgen identified the X-ray, Tesla began making X-ray images of his own using high voltages and tubes of his own design,[13] as well as Crookes tubes.
Discovery by Röntgen[edit]
On November 8, 1895, German physics professor Wilhelm Röntgen stumbled on X-rays while experimenting with Lenard tubes and Crookes tubes and began studying them. He wrote an initial report «On a new kind of ray: A preliminary communication» and on December 28, 1895, submitted it to Würzburg’s Physical-Medical Society journal.[14] This was the first paper written on X-rays. Röntgen referred to the radiation as «X», to indicate that it was an unknown type of radiation. Some early texts refer to them as Chi-rays having interpreted «X» as the uppercase Greek letter Chi, Χ.[15][16][17] The name X-rays stuck, although (over Röntgen’s great objections) many of his colleagues suggested calling them Röntgen rays. They are still referred to as such in many languages, including German, Hungarian, Ukrainian, Danish, Polish, Czech, Bulgarian, Swedish, Finnish, Estonian, Slovenian, Turkish, Russian, Latvian, Lithuanian, Albanian, Japanese, Dutch, Georgian, Hebrew, and Norwegian. Röntgen received the first Nobel Prize in Physics for his discovery.[18]
There are conflicting accounts of his discovery because Röntgen had his lab notes burned after his death, but this is a likely reconstruction by his biographers:[19][20] Röntgen was investigating cathode rays from a Crookes tube which he had wrapped in black cardboard so that the visible light from the tube would not interfere, using a fluorescent screen painted with barium platinocyanide. He noticed a faint green glow from the screen, about 1 meter (3.3 ft) away. Röntgen realized some invisible rays coming from the tube were passing through the cardboard to make the screen glow. He found they could also pass through books and papers on his desk. Röntgen threw himself into investigating these unknown rays systematically. Two months after his initial discovery, he published his paper.[21]
Röntgen discovered their medical use when he made a picture of his wife’s hand on a photographic plate formed due to X-rays. The photograph of his wife’s hand was the first photograph of a human body part using X-rays. When she saw the picture, she said «I have seen my death.»[24]
The discovery of X-rays stimulated a veritable sensation. Röntgen’s biographer Otto Glasser estimated that, in 1896 alone, as many as 49 essays and 1044 articles about the new rays were published.[25] This was probably a conservative estimate, if one considers that nearly every paper around the world extensively reported about the new discovery, with a magazine such as Science dedicating as many as 23 articles to it in that year alone.[26] Sensationalist reactions to the new discovery included publications linking the new kind of rays to occult and paranormal theories, such as telepathy.[27][28]
Advances in radiology[edit]
Taking an X-ray image with early Crookes tube apparatus, late 1800s. The Crookes tube is visible in center. The standing man is viewing his hand with a fluoroscope screen. The seated man is taking a radiograph of his hand by placing it on a photographic plate. No precautions against radiation exposure are taken; its hazards were not known at the time.
Surgical removal of a bullet whose location was diagnosed with X-rays (see inset) in 1897
Röntgen immediately noticed X-rays could have medical applications. Along with his 28 December Physical-Medical Society submission, he sent a letter to physicians he knew around Europe (January 1, 1896).[29] News (and the creation of «shadowgrams») spread rapidly with Scottish electrical engineer Alan Archibald Campbell-Swinton being the first after Röntgen to create an X-ray (of a hand). Through February, there were 46 experimenters taking up the technique in North America alone.[29]
The first use of X-rays under clinical conditions was by John Hall-Edwards in Birmingham, England on 11 January 1896, when he radiographed a needle stuck in the hand of an associate. On February 14, 1896, Hall-Edwards was also the first to use X-rays in a surgical operation.[30]
In early 1896, several weeks after Röntgen’s discovery, Ivan Romanovich Tarkhanov irradiated frogs and insects with X-rays, concluding that the rays «not only photograph, but also affect the living function».[31] At around the same time, the zoological illustrator James Green began to use X-rays to examine fragile specimens. George Albert Boulenger first mentioned this work in a paper he delivered before the Zoological Society of London in May 1896. The book Sciagraphs of British Batrachians and Reptiles (sciagraph is an obsolete name for an X-ray photograph), by Green and James H. Gardiner, with a foreword by Boulenger, was published in 1897.[32][33]
The first medical X-ray made in the United States was obtained using a discharge tube of Pului’s design. In January 1896, on reading of Röntgen’s discovery, Frank Austin of Dartmouth College tested all of the discharge tubes in the physics laboratory and found that only the Pului tube produced X-rays. This was a result of Pului’s inclusion of an oblique «target» of mica, used for holding samples of fluorescent material, within the tube. On 3 February 1896, Gilman Frost, professor of medicine at the college, and his brother Edwin Frost, professor of physics, exposed the wrist of Eddie McCarthy, whom Gilman had treated some weeks earlier for a fracture, to the X-rays and collected the resulting image of the broken bone on gelatin photographic plates obtained from Howard Langill, a local photographer also interested in Röntgen’s work.[34]
1896 plaque published in «Nouvelle Iconographie de la Salpetrière», a medical journal. In the left a hand deformity, in the right same hand seen using radiography. The authors named the technique Röntgen photography.
Many experimenters, including Röntgen himself in his original experiments, came up with methods to view X-ray images «live» using some form of luminescent screen.[29] Röntgen used a screen coated with barium platinocyanide. On February 5, 1896, live imaging devices were developed by both Italian scientist Enrico Salvioni (his «cryptoscope») and Professor McGie of Princeton University (his «Skiascope»), both using barium platinocyanide. American inventor Thomas Edison started research soon after Röntgen’s discovery and investigated materials’ ability to fluoresce when exposed to X-rays, finding that calcium tungstate was the most effective substance. In May 1896, he developed the first mass-produced live imaging device, his «Vitascope», later called the fluoroscope, which became the standard for medical X-ray examinations.[29] Edison dropped X-ray research around 1903, before the death of Clarence Madison Dally, one of his glassblowers. Dally had a habit of testing X-ray tubes on his own hands, developing a cancer in them so tenacious that both arms were amputated in a futile attempt to save his life; in 1904, he became the first known death attributed to X-ray exposure.[29] During the time the fluoroscope was being developed, Serbian American physicist Mihajlo Pupin, using a calcium tungstate screen developed by Edison, found that using a fluorescent screen decreased the exposure time it took to create an X-ray for medical imaging from an hour to a few minutes.[35][29]
In 1901, U.S. President William McKinley was shot twice in an assassination attempt while attending the Pan American Exposition in Buffalo, New York. While one bullet only grazed his sternum, another had lodged somewhere deep inside his abdomen and could not be found. A worried McKinley aide sent word to inventor Thomas Edison to rush an X-ray machine to Buffalo to find the stray bullet. It arrived but was not used. While the shooting itself had not been lethal, gangrene had developed along the path of the bullet, and McKinley died of septic shock due to bacterial infection six days later.[36]
Hazards discovered[edit]
With the widespread experimentation with X‑rays after their discovery in 1895 by scientists, physicians, and inventors came many stories of burns, hair loss, and worse in technical journals of the time. In February 1896, Professor John Daniel and Dr. William Lofland Dudley of Vanderbilt University reported hair loss after Dr. Dudley was X-rayed. A child who had been shot in the head was brought to the Vanderbilt laboratory in 1896. Before trying to find the bullet, an experiment was attempted, for which Dudley «with his characteristic devotion to science»[37][38][39] volunteered. Daniel reported that 21 days after taking a picture of Dudley’s skull (with an exposure time of one hour), he noticed a bald spot 5 centimeters (2 in) in diameter on the part of his head nearest the X-ray tube: «A plate holder with the plates towards the side of the skull was fastened and a coin placed between the skull and the head. The tube was fastened at the other side at a distance of one-half inch [1.3 cm] from the hair.»[40]
In August 1896, Dr. HD. Hawks, a graduate of Columbia College, suffered severe hand and chest burns from an X-ray demonstration. It was reported in Electrical Review and led to many other reports of problems associated with X-rays being sent in to the publication.[41] Many experimenters including Elihu Thomson at Edison’s lab, William J. Morton, and Nikola Tesla also reported burns. Elihu Thomson deliberately exposed a finger to an X-ray tube over a period of time and suffered pain, swelling, and blistering.[42] Other effects were sometimes blamed for the damage including ultraviolet rays and (according to Tesla) ozone.[11] Many physicians claimed there were no effects from X-ray exposure at all.[42] On August 3, 1905, in San Francisco, California, Elizabeth Fleischman, an American X-ray pioneer, died from complications as a result of her work with X-rays.[43][44][45]
Hall-Edwards developed a cancer (then called X-ray dermatitis) sufficiently advanced by 1904 to cause him to write papers and give public addresses on the dangers of X-rays. His left arm had to be amputated at the elbow in 1908,[46] and four fingers on his right arm soon thereafter, leaving only a thumb. He died of cancer in 1926. His left hand is kept at Birmingham University.
20th century and beyond[edit]
A patient being examined with a thoracic fluoroscope in 1940, which displayed continuous moving images. This image was used to argue that radiation exposure during the X-ray procedure would be negligible.
The many applications of X-rays immediately generated enormous interest. Workshops began making specialized versions of Crookes tubes for generating X-rays and these first-generation cold cathode or Crookes X-ray tubes were used until about 1920.
A typical early 20th century medical X-ray system consisted of a Ruhmkorff coil connected to a cold cathode Crookes X-ray tube. A spark gap was typically connected to the high voltage side in parallel to the tube and used for diagnostic purposes.[47] The spark gap allowed detecting the polarity of the sparks, measuring voltage by the length of the sparks thus determining the «hardness» of the vacuum of the tube, and it provided a load in the event the X-ray tube was disconnected. To detect the hardness of the tube, the spark gap was initially opened to the widest setting. While the coil was operating, the operator reduced the gap until sparks began to appear. A tube in which the spark gap began to spark at around 6.4 centimeters (2.5 in) was considered soft (low vacuum) and suitable for thin body parts such as hands and arms. A 13-centimeter (5 in) spark indicated the tube was suitable for shoulders and knees. An 18-to-23-centimeter (7 to 9 in) spark would indicate a higher vacuum suitable for imaging the abdomen of larger individuals. Since the spark gap was connected in parallel to the tube, the spark gap had to be opened until the sparking ceased in order to operate the tube for imaging. Exposure time for photographic plates was around half a minute for a hand to a couple of minutes for a thorax. The plates may have a small addition of fluorescent salt to reduce exposure times.[47]
Crookes tubes were unreliable. They had to contain a small quantity of gas (invariably air) as a current will not flow in such a tube if they are fully evacuated. However, as time passed, the X-rays caused the glass to absorb the gas, causing the tube to generate «harder» X-rays until it soon stopped operating. Larger and more frequently used tubes were provided with devices for restoring the air, known as «softeners». These often took the form of a small side tube that contained a small piece of mica, a mineral that traps relatively large quantities of air within its structure. A small electrical heater heated the mica, causing it to release a small amount of air, thus restoring the tube’s efficiency. However, the mica had a limited life, and the restoration process was difficult to control.
In 1904, John Ambrose Fleming invented the thermionic diode, the first kind of vacuum tube. This used a hot cathode that caused an electric current to flow in a vacuum. This idea was quickly applied to X-ray tubes, and hence heated-cathode X-ray tubes, called «Coolidge tubes», completely replaced the troublesome cold cathode tubes by about 1920.
In about 1906, the physicist Charles Barkla discovered that X-rays could be scattered by gases, and that each element had a characteristic X-ray spectrum. He won the 1917 Nobel Prize in Physics for this discovery.
In 1912, Max von Laue, Paul Knipping, and Walter Friedrich first observed the diffraction of X-rays by crystals. This discovery, along with the early work of Paul Peter Ewald, William Henry Bragg, and William Lawrence Bragg, gave birth to the field of X-ray crystallography.[48]
In 1913, Henry Moseley performed crystallography experiments with X-rays emanating from various metals and formulated Moseley’s law which relates the frequency of the X-rays to the atomic number of the metal.
The Coolidge X-ray tube was invented the same year by William D. Coolidge. It made possible the continuous emissions of X-rays. Modern X-ray tubes are based on this design, often employing the use of rotating targets which allow for significantly higher heat dissipation than static targets, further allowing higher quantity X-ray output for use in high powered applications such as rotational CT scanners.
Chandra’s image of the galaxy cluster Abell 2125 reveals a complex of several massive multimillion-degree-Celsius gas clouds in the process of merging.
The use of X-rays for medical purposes (which developed into the field of radiation therapy) was pioneered by Major John Hall-Edwards in Birmingham, England. Then in 1908, he had to have his left arm amputated because of the spread of X-ray dermatitis on his arm.[49]
Medical science also used the motion picture to study human physiology. In 1913, a motion picture was made in Detroit showing a hard-boiled egg inside a human stomach. This early X-ray movie was recorded at a rate of one still image every four seconds.[50] Dr Lewis Gregory Cole of New York was a pioneer of the technique, which he called «serial radiography».[51][52] In 1918, X-rays were used in association with motion picture cameras to capture the human skeleton in motion.[53][54][55] In 1920, it was used to record the movements of tongue and teeth in the study of languages by the Institute of Phonetics in England.[56]
In 1914, Marie Curie developed radiological cars to support soldiers injured in World War I. The cars would allow for rapid X-ray imaging of wounded soldiers so battlefield surgeons could quickly and more accurately operate.[57]
From the early 1920s through to the 1950s, X-ray machines were developed to assist in the fitting of shoes[58] and were sold to commercial shoe stores.[59][60][61] Concerns regarding the impact of frequent or poorly controlled use were expressed in the 1950s,[62][63] leading to the practice’s eventual end that decade.[64]
The X-ray microscope was developed during the 1950s.
The Chandra X-ray Observatory, launched on July 23, 1999, has been allowing the exploration of the very violent processes in the universe which produce X-rays. Unlike visible light, which gives a relatively stable view of the universe, the X-ray universe is unstable. It features stars being torn apart by black holes, galactic collisions, and novae, and neutron stars that build up layers of plasma that then explode into space.
Phase-contrast X-ray image of a spider
An X-ray laser device was proposed as part of the Reagan Administration’s Strategic Defense Initiative in the 1980s, but the only test of the device (a sort of laser «blaster» or death ray, powered by a thermonuclear explosion) gave inconclusive results. For technical and political reasons, the overall project (including the X-ray laser) was defunded (though was later revived by the second Bush Administration as National Missile Defense using different technologies).
Phase-contrast X-ray imaging refers to a variety of techniques that use phase information of an X-ray beam to form the image. Due to its good sensitivity to density differences, it is especially useful for imaging soft tissues. It has become an important method for visualizing cellular and histological structures in a wide range of biological and medical studies. There are several technologies being used for X-ray phase-contrast imaging, all utilizing different principles to convert phase variations in the X-rays emerging from an object into intensity variations.[65][66] These include propagation-based phase contrast,[67] Talbot interferometry,[66] refraction-enhanced imaging,[68] and X-ray interferometry.[69] These methods provide higher contrast compared to normal absorption-based X-ray imaging, making it possible to distinguish from each other details that have almost similar density. A disadvantage is that these methods require more sophisticated equipment, such as synchrotron or microfocus X-ray sources, X-ray optics, and high resolution X-ray detectors.
Energy ranges[edit]
Soft and hard X-rays[edit]
X-rays with high photon energies above 5–10 keV (below 0.2–0.1 nm wavelength) are called hard X-rays, while those with lower energy (and longer wavelength) are called soft X-rays.[70] The intermediate range with photon energies of several keV is often referred to as tender X-rays. Due to their penetrating ability, hard X-rays are widely used to image the inside of objects, e.g., in medical radiography and airport security. The term X-ray is metonymically used to refer to a radiographic image produced using this method, in addition to the method itself. Since the wavelengths of hard X-rays are similar to the size of atoms, they are also useful for determining crystal structures by X-ray crystallography. By contrast, soft X-rays are easily absorbed in air; the attenuation length of 600 eV (~2 nm) X-rays in water is less than 1 micrometer.[71]
Gamma rays[edit]
There is no consensus for a definition distinguishing between X-rays and gamma rays. One common practice is to distinguish between the two types of radiation based on their source: X-rays are emitted by electrons, while gamma rays are emitted by the atomic nucleus.[72][73][74][75] This definition has several problems: other processes can also generate these high-energy photons, or sometimes the method of generation is not known. One common alternative is to distinguish X- and gamma radiation on the basis of wavelength (or, equivalently, frequency or photon energy), with radiation shorter than some arbitrary wavelength, such as 10−11 m (0.1 Å), defined as gamma radiation.[76] This criterion assigns a photon to an unambiguous category, but is only possible if wavelength is known. (Some measurement techniques do not distinguish between detected wavelengths.) However, these two definitions often coincide since the electromagnetic radiation emitted by X-ray tubes generally has a longer wavelength and lower photon energy than the radiation emitted by radioactive nuclei.[72] Occasionally, one term or the other is used in specific contexts due to historical precedent, based on measurement (detection) technique, or based on their intended use rather than their wavelength or source.
Thus, gamma-rays generated for medical and industrial uses, for example radiotherapy, in the ranges of 6–20 MeV, can in this context also be referred to as X-rays.[77]
Properties[edit]
Ionizing radiation hazard symbol
X-ray photons carry enough energy to ionize atoms and disrupt molecular bonds. This makes it a type of ionizing radiation, and therefore harmful to living tissue. A very high radiation dose over a short period of time causes radiation sickness, while lower doses can give an increased risk of radiation-induced cancer. In medical imaging, this increased cancer risk is generally greatly outweighed by the benefits of the examination. The ionizing capability of X-rays can be utilized in cancer treatment to kill malignant cells using radiation therapy. It is also used for material characterization using X-ray spectroscopy.
Hard X-rays can traverse relatively thick objects without being much absorbed or scattered. For this reason, X-rays are widely used to image the inside of visually opaque objects. The most often seen applications are in medical radiography and airport security scanners, but similar techniques are also important in industry (e.g., industrial radiography and industrial CT scanning) and research (e.g., small animal CT). The penetration depth varies with several orders of magnitude over the X-ray spectrum. This allows the photon energy to be adjusted for the application so as to give sufficient transmission through the object and at the same time provide good contrast in the image.
X-rays have much shorter wavelengths than visible light, which makes it possible to probe structures much smaller than can be seen using a normal microscope. This property is used in X-ray microscopy to acquire high-resolution images, and also in X-ray crystallography to determine the positions of atoms in crystals.
Interaction with matter[edit]
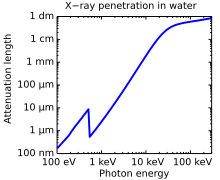
Attenuation length of X-rays in water showing the oxygen absorption edge at 540 eV, the energy−3 dependence of photoabsorption, as well as a leveling off at higher photon energies due to Compton scattering. The attenuation length is about four orders of magnitude longer for hard X-rays (right half) compared to soft X-rays (left half).
X-rays interact with matter in three main ways, through photoabsorption, Compton scattering, and Rayleigh scattering. The strength of these interactions depends on the energy of the X-rays and the elemental composition of the material, but not much on chemical properties, since the X-ray photon energy is much higher than chemical binding energies. Photoabsorption or photoelectric absorption is the dominant interaction mechanism in the soft X-ray regime and for the lower hard X-ray energies. At higher energies, Compton scattering dominates.
Photoelectric absorption[edit]
The probability of a photoelectric absorption per unit mass is approximately proportional to Z3/E3, where Z is the atomic number and E is the energy of the incident photon.[78] This rule is not valid close to inner shell electron binding energies where there are abrupt changes in interaction probability, so called absorption edges. However, the general trend of high absorption coefficients and thus short penetration depths for low photon energies and high atomic numbers is very strong. For soft tissue, photoabsorption dominates up to about 26 keV photon energy where Compton scattering takes over. For higher atomic number substances, this limit is higher. The high amount of calcium (Z = 20) in bones, together with their high density, is what makes them show up so clearly on medical radiographs.
A photoabsorbed photon transfers all its energy to the electron with which it interacts, thus ionizing the atom to which the electron was bound and producing a photoelectron that is likely to ionize more atoms in its path. An outer electron will fill the vacant electron position and produce either a characteristic X-ray or an Auger electron. These effects can be used for elemental detection through X-ray spectroscopy or Auger electron spectroscopy.
Compton scattering[edit]
Compton scattering is the predominant interaction between X-rays and soft tissue in medical imaging.[79] Compton scattering is an inelastic scattering of the X-ray photon by an outer shell electron. Part of the energy of the photon is transferred to the scattering electron, thereby ionizing the atom and increasing the wavelength of the X-ray. The scattered photon can go in any direction, but a direction similar to the original direction is more likely, especially for high-energy X-rays. The probability for different scattering angles is described by the Klein–Nishina formula. The transferred energy can be directly obtained from the scattering angle from the conservation of energy and momentum.
Rayleigh scattering[edit]
Rayleigh scattering is the dominant elastic scattering mechanism in the X-ray regime.[80] Inelastic forward scattering gives rise to the refractive index, which for X-rays is only slightly below 1.[81]
Production[edit]
Whenever charged particles (electrons or ions) of sufficient energy hit a material, X-rays are produced.
Production by electrons[edit]
| Anode material |
Atomic number |
Photon energy [keV] | Wavelength [nm] | ||
|---|---|---|---|---|---|
| Kα1 | Kβ1 | Kα1 | Kβ1 | ||
| W | 74 | 59.3 | 67.2 | 0.0209 | 0.0184 |
| Mo | 42 | 17.5 | 19.6 | 0.0709 | 0.0632 |
| Cu | 29 | 8.05 | 8.91 | 0.154 | 0.139 |
| Ag | 47 | 22.2 | 24.9 | 0.0559 | 0.0497 |
| Ga | 31 | 9.25 | 10.26 | 0.134 | 0.121 |
| In | 49 | 24.2 | 27.3 | 0.0512 | 0.0455 |
X-rays can be generated by an X-ray tube, a vacuum tube that uses a high voltage to accelerate the electrons released by a hot cathode to a high velocity. The high velocity electrons collide with a metal target, the anode, creating the X-rays.[84] In medical X-ray tubes the target is usually tungsten or a more crack-resistant alloy of rhenium (5%) and tungsten (95%), but sometimes molybdenum for more specialized applications, such as when softer X-rays are needed as in mammography. In crystallography, a copper target is most common, with cobalt often being used when fluorescence from iron content in the sample might otherwise present a problem.
The maximum energy of the produced X-ray photon is limited by the energy of the incident electron, which is equal to the voltage on the tube times the electron charge, so an 80 kV tube cannot create X-rays with an energy greater than 80 keV. When the electrons hit the target, X-rays are created by two different atomic processes:
- Characteristic X-ray emission (X-ray electroluminescence): If the electron has enough energy, it can knock an orbital electron out of the inner electron shell of the target atom. After that, electrons from higher energy levels fill the vacancies, and X-ray photons are emitted. This process produces an emission spectrum of X-rays at a few discrete frequencies, sometimes referred to as spectral lines. Usually, these are transitions from the upper shells to the K shell (called K lines), to the L shell (called L lines) and so on. If the transition is from 2p to 1s, it is called Kα, while if it is from 3p to 1s it is Kβ. The frequencies of these lines depend on the material of the target and are therefore called characteristic lines. The Kα line usually has greater intensity than the Kβ one and is more desirable in diffraction experiments. Thus the Kβ line is filtered out by a filter. The filter is usually made of a metal having one proton less than the anode material (e.g., Ni filter for Cu anode or Nb filter for Mo anode).
- Bremsstrahlung: This is radiation given off by the electrons as they are scattered by the strong electric field near the high-Z (proton number) nuclei. These X-rays have a continuous spectrum. The frequency of Bremsstrahlung is limited by the energy of incident electrons.
So, the resulting output of a tube consists of a continuous Bremsstrahlung spectrum falling off to zero at the tube voltage, plus several spikes at the characteristic lines. The voltages used in diagnostic X-ray tubes range from roughly 20 kV to 150 kV and thus the highest energies of the X-ray photons range from roughly 20 keV to 150 keV.[85]
Both of these X-ray production processes are inefficient, with only about one percent of the electrical energy used by the tube converted into X-rays, and thus most of the electric power consumed by the tube is released as waste heat. When producing a usable flux of X-rays, the X-ray tube must be designed to dissipate the excess heat.
A specialized source of X-rays which is becoming widely used in research is synchrotron radiation, which is generated by particle accelerators. Its unique features are X-ray outputs many orders of magnitude greater than those of X-ray tubes, wide X-ray spectra, excellent collimation, and linear polarization.[86]
Short nanosecond bursts of X-rays peaking at 15 keV in energy may be reliably produced by peeling pressure-sensitive adhesive tape from its backing in a moderate vacuum. This is likely to be the result of recombination of electrical charges produced by triboelectric charging. The intensity of X-ray triboluminescence is sufficient for it to be used as a source for X-ray imaging.[87]
Production by fast positive ions[edit]
X-rays can also be produced by fast protons or other positive ions. The proton-induced X-ray emission or particle-induced X-ray emission is widely used as an analytical procedure. For high energies, the production cross section is proportional to Z12Z2−4, where Z1 refers to the atomic number of the ion, Z2 refers to that of the target atom.[88] An overview of these cross sections is given in the same reference.
Production in lightning and laboratory discharges[edit]
X-rays are also produced in lightning accompanying terrestrial gamma-ray flashes. The underlying mechanism is the acceleration of electrons in lightning related electric fields and the subsequent production of photons through Bremsstrahlung.[89] This produces photons with energies of some few keV and several tens of MeV.[90] In laboratory discharges with a gap size of approximately 1 meter length and a peak voltage of 1 MV, X-rays with a characteristic energy of 160 keV are observed.[91] A possible explanation is the encounter of two streamers and the production of high-energy run-away electrons;[92] however, microscopic simulations have shown that the duration of electric field enhancement between two streamers is too short to produce a significant number of run-away electrons.[93] Recently, it has been proposed that air perturbations in the vicinity of streamers can facilitate the production of run-away electrons and hence of X-rays from discharges.[94][95]
Detectors[edit]
X-ray detectors vary in shape and function depending on their purpose. Imaging detectors such as those used for radiography were originally based on photographic plates and later photographic film, but are now mostly replaced by various digital detector types such as image plates and flat panel detectors. For radiation protection direct exposure hazard is often evaluated using ionization chambers, while dosimeters are used to measure the radiation dose a person has been exposed to. X-ray spectra can be measured either by energy dispersive or wavelength dispersive spectrometers. For X-ray diffraction applications, such as X-ray crystallography, hybrid photon counting detectors are widely used.[96]
Medical uses[edit]
Patient undergoing an x-ray exam in a hospital radiology room.
Since Röntgen’s discovery that X-rays can identify bone structures, X-rays have been used for medical imaging.[97] The first medical use was less than a month after his paper on the subject.[34] Up to 2010, five billion medical imaging examinations had been conducted worldwide.[98] Radiation exposure from medical imaging in 2006 made up about 50% of total ionizing radiation exposure in the United States.[99]
Projectional radiographs[edit]
Plain radiograph of the right knee
Projectional radiography is the practice of producing two-dimensional images using X-ray radiation. Bones contain a high concentration of calcium, which, due to its relatively high atomic number, absorbs X-rays efficiently. This reduces the amount of X-rays reaching the detector in the shadow of the bones, making them clearly visible on the radiograph. The lungs and trapped gas also show up clearly because of lower absorption compared to tissue, while differences between tissue types are harder to see.
Projectional radiographs are useful in the detection of pathology of the skeletal system as well as for detecting some disease processes in soft tissue. Some notable examples are the very common chest X-ray, which can be used to identify lung diseases such as pneumonia, lung cancer, or pulmonary edema, and the abdominal x-ray, which can detect bowel (or intestinal) obstruction, free air (from visceral perforations), and free fluid (in ascites). X-rays may also be used to detect pathology such as gallstones (which are rarely radiopaque) or kidney stones which are often (but not always) visible. Traditional plain X-rays are less useful in the imaging of soft tissues such as the brain or muscle. One area where projectional radiographs are used extensively is in evaluating how an orthopedic implant, such as a knee, hip or shoulder replacement, is situated in the body with respect to the surrounding bone. This can be assessed in two dimensions from plain radiographs, or it can be assessed in three dimensions if a technique called ‘2D to 3D registration’ is used. This technique purportedly negates projection errors associated with evaluating implant position from plain radiographs.[100]
Dental radiography is commonly used in the diagnoses of common oral problems, such as cavities.
In medical diagnostic applications, the low energy (soft) X-rays are unwanted, since they are totally absorbed by the body, increasing the radiation dose without contributing to the image. Hence, a thin metal sheet, often of aluminium, called an X-ray filter, is usually placed over the window of the X-ray tube, absorbing the low energy part in the spectrum. This is called hardening the beam since it shifts the center of the spectrum towards higher energy (or harder) X-rays.
To generate an image of the cardiovascular system, including the arteries and veins (angiography) an initial image is taken of the anatomical region of interest. A second image is then taken of the same region after an iodinated contrast agent has been injected into the blood vessels within this area. These two images are then digitally subtracted, leaving an image of only the iodinated contrast outlining the blood vessels. The radiologist or surgeon then compares the image obtained to normal anatomical images to determine whether there is any damage or blockage of the vessel.
Computed tomography[edit]
Computed tomography (CT scanning) is a medical imaging modality where tomographic images or slices of specific areas of the body are obtained from a large series of two-dimensional X-ray images taken in different directions.[101] These cross-sectional images can be combined into a three-dimensional image of the inside of the body and used for diagnostic and therapeutic purposes in various medical disciplines.
Fluoroscopy[edit]
Fluoroscopy is an imaging technique commonly used by physicians or radiation therapists to obtain real-time moving images of the internal structures of a patient through the use of a fluoroscope. In its simplest form, a fluoroscope consists of an X-ray source and a fluorescent screen, between which a patient is placed. However, modern fluoroscopes couple the screen to an X-ray image intensifier and CCD video camera allowing the images to be recorded and played on a monitor. This method may use a contrast material. Examples include cardiac catheterization (to examine for coronary artery blockages) and barium swallow (to examine for esophageal disorders and swallowing disorders).
Radiotherapy[edit]
The use of X-rays as a treatment is known as radiation therapy and is largely used for the management (including palliation) of cancer; it requires higher radiation doses than those received for imaging alone. X-rays beams are used for treating skin cancers using lower energy X-ray beams while higher energy beams are used for treating cancers within the body such as brain, lung, prostate, and breast.[102][103]
Adverse effects[edit]
Abdominal radiograph of a pregnant woman, a procedure that should be performed only after proper assessment of benefit versus risk
Diagnostic X-rays (primarily from CT scans due to the large dose used) increase the risk of developmental problems and cancer in those exposed.[104][105][106] X-rays are classified as a carcinogen by both the World Health Organization’s International Agency for Research on Cancer and the U.S. government.[98][107] It is estimated that 0.4% of current cancers in the United States are due to computed tomography (CT scans) performed in the past and that this may increase to as high as 1.5–2% with 2007 rates of CT usage.[108]
Experimental and epidemiological data currently do not support the proposition that there is a threshold dose of radiation below which there is no increased risk of cancer.[109] However, this is under increasing doubt.[110] Cancer risk can start at the exposure of 1100 mGy.[111] It is estimated that the additional radiation from diagnostic X-rays will increase the average person’s cumulative risk of getting cancer by age 75 by 0.6–3.0%.[112] The amount of absorbed radiation depends upon the type of X-ray test and the body part involved.[108] CT and fluoroscopy entail higher doses of radiation than do plain X-rays.
To place the increased risk in perspective, a plain chest X-ray will expose a person to the same amount from background radiation that people are exposed to (depending upon location) every day over 10 days, while exposure from a dental X-ray is approximately equivalent to 1 day of environmental background radiation.[113] Each such X-ray would add less than 1 per 1,000,000 to the lifetime cancer risk. An abdominal or chest CT would be the equivalent to 2–3 years of background radiation to the whole body, or 4–5 years to the abdomen or chest, increasing the lifetime cancer risk between 1 per 1,000 to 1 per 10,000.[113] This is compared to the roughly 40% chance of a US citizen developing cancer during their lifetime.[114] For instance, the effective dose to the torso from a CT scan of the chest is about 5 mSv, and the absorbed dose is about 14 mGy.[115] A head CT scan (1.5 mSv, 64 mGy)[116] that is performed once with and once without contrast agent, would be equivalent to 40 years of background radiation to the head. Accurate estimation of effective doses due to CT is difficult with the estimation uncertainty range of about ±19% to ±32% for adult head scans depending upon the method used.[117]
The risk of radiation is greater to a fetus, so in pregnant patients, the benefits of the investigation (X-ray) should be balanced with the potential hazards to the fetus.[118][119] If there is 1 scan in 9 months, it can be harmful to the fetus.[120] Therefore, women who are pregnant get ultrasounds as their diagnostic imaging because this does not use radiation.[120] If there is too much radiation exposure there could be harmful effects on the fetus or the reproductive organs of the mother.[120] In the US, there are an estimated 62 million CT scans performed annually, including more than 4 million on children.[108] Avoiding unnecessary X-rays (especially CT scans) reduces radiation dose and any associated cancer risk.[121]
Medical X-rays are a significant source of human-made radiation exposure. In 1987, they accounted for 58% of exposure from human-made sources in the United States. Since human-made sources accounted for only 18% of the total radiation exposure, most of which came from natural sources (82%), medical X-rays only accounted for 10% of total American radiation exposure; medical procedures as a whole (including nuclear medicine) accounted for 14% of total radiation exposure. By 2006, however, medical procedures in the United States were contributing much more ionizing radiation than was the case in the early 1980s. In 2006, medical exposure constituted nearly half of the total radiation exposure of the U.S. population from all sources. The increase is traceable to the growth in the use of medical imaging procedures, in particular computed tomography (CT), and to the growth in the use of nuclear medicine.[99][122]
Dosage due to dental X-rays varies significantly depending on the procedure and the technology (film or digital). Depending on the procedure and the technology, a single dental X-ray of a human results in an exposure of 0.5 to 4 mrem. A full mouth series of X-rays may result in an exposure of up to 6 (digital) to 18 (film) mrem, for a yearly average of up to 40 mrem.[123][124][125][126][127][128][129]
Financial incentives have been shown to have a significant impact on X-ray use with doctors who are paid a separate fee for each X-ray providing more X-rays.[130]
Early photon tomography or EPT[131] (as of 2015) along with other techniques[132] are being researched as potential alternatives to X-rays for imaging applications.
Other uses[edit]
Other notable uses of X-rays include:
Each dot, called a reflection, in this diffraction pattern forms from the constructive interference of scattered X-rays passing through a crystal. The data can be used to determine the crystalline structure.
- X-ray crystallography in which the pattern produced by the diffraction of X-rays through the closely spaced lattice of atoms in a crystal is recorded and then analysed to reveal the nature of that lattice. A related technique, fiber diffraction, was used by Rosalind Franklin to discover the double helical structure of DNA.[133]
- X-ray astronomy, which is an observational branch of astronomy, which deals with the study of X-ray emission from celestial objects.
- X-ray microscopic analysis, which uses electromagnetic radiation in the soft X-ray band to produce images of very small objects.
- X-ray fluorescence, a technique in which X-rays are generated within a specimen and detected. The outgoing energy of the X-ray can be used to identify the composition of the sample.
- Industrial radiography uses X-rays for inspection of industrial parts, particularly welds.
- Radiography of cultural objects, most often x-rays of paintings to reveal underdrawing, pentimenti alterations in the course of painting or by later restorers, and sometimes previous paintings on the support. Many pigments such as lead white show well in radiographs.
- X-ray spectromicroscopy has been used to analyse the reactions of pigments in paintings. For example, in analysing colour degradation in the paintings of van Gogh.[134]
Using X-ray for inspection and quality control: the differences in the structures of the die and bond wires reveal the left chip to be counterfeit.[135]
- Authentication and quality control of packaged items.
- Industrial CT (computed tomography), a process that uses X-ray equipment to produce three-dimensional representations of components both externally and internally. This is accomplished through computer processing of projection images of the scanned object in many directions.
- Airport security luggage scanners use X-rays for inspecting the interior of luggage for security threats before loading on aircraft.
- Border control truck scanners and domestic police departments use X-rays for inspecting the interior of trucks.
- X-ray art and fine art photography, artistic use of X-rays, for example the works by Stane Jagodič
- X-ray hair removal, a method popular in the 1920s but now banned by the FDA.[136]
- Shoe-fitting fluoroscopes were popularized in the 1920s, banned in the US in the 1960s, in the UK in the 1970s, and later in continental Europe.
- Roentgen stereophotogrammetry is used to track movement of bones based on the implantation of markers
- X-ray photoelectron spectroscopy is a chemical analysis technique relying on the photoelectric effect, usually employed in surface science.
- Radiation implosion is the use of high energy X-rays generated from a fission explosion (an A-bomb) to compress nuclear fuel to the point of fusion ignition (an H-bomb).
Visibility[edit]
While generally considered invisible to the human eye, in special circumstances X-rays can be visible. Brandes, in an experiment a short time after Röntgen’s landmark 1895 paper, reported after dark adaptation and placing his eye close to an X-ray tube, seeing a faint «blue-gray» glow which seemed to originate within the eye itself.[137] Upon hearing this, Röntgen reviewed his record books and found he too had seen the effect. When placing an X-ray tube on the opposite side of a wooden door Röntgen had noted the same blue glow, seeming to emanate from the eye itself, but thought his observations to be spurious because he only saw the effect when he used one type of tube. Later he realized that the tube which had created the effect was the only one powerful enough to make the glow plainly visible and the experiment was thereafter readily repeatable. The knowledge that X-rays are actually faintly visible to the dark-adapted naked eye has largely been forgotten today; this is probably due to the desire not to repeat what would now be seen as a recklessly dangerous and potentially harmful experiment with ionizing radiation. It is not known what exact mechanism in the eye produces the visibility: it could be due to conventional detection (excitation of rhodopsin molecules in the retina), direct excitation of retinal nerve cells, or secondary detection via, for instance, X-ray induction of phosphorescence in the eyeball with conventional retinal detection of the secondarily produced visible light.
Though X-rays are otherwise invisible, it is possible to see the ionization of the air molecules if the intensity of the X-ray beam is high enough. The beamline from the wiggler at the European Synchrotron Radiation Facility[138] is one example of such high intensity.[139]
Units of measure and exposure[edit]
The measure of X-rays ionizing ability is called the exposure:
- The coulomb per kilogram (C/kg) is the SI unit of ionizing radiation exposure, and it is the amount of radiation required to create one coulomb of charge of each polarity in one kilogram of matter.
- The roentgen (R) is an obsolete traditional unit of exposure, which represented the amount of radiation required to create one electrostatic unit of charge of each polarity in one cubic centimeter of dry air. 1 roentgen = 2.58×10−4 C/kg.
However, the effect of ionizing radiation on matter (especially living tissue) is more closely related to the amount of energy deposited into them rather than the charge generated. This measure of energy absorbed is called the absorbed dose:
- The gray (Gy), which has units of (joules/kilogram), is the SI unit of absorbed dose, and it is the amount of radiation required to deposit one joule of energy in one kilogram of any kind of matter.
- The rad is the (obsolete) corresponding traditional unit, equal to 10 millijoules of energy deposited per kilogram. 100 rad = 1 gray.
The equivalent dose is the measure of the biological effect of radiation on human tissue. For X-rays it is equal to the absorbed dose.
- The Roentgen equivalent man (rem) is the traditional unit of equivalent dose. For X-rays it is equal to the rad, or, in other words, 10 millijoules of energy deposited per kilogram. 100 rem = 1 Sv.
- The sievert (Sv) is the SI unit of equivalent dose, and also of effective dose. For X-rays the «equivalent dose» is numerically equal to a Gray (Gy). 1 Sv = 1 Gy. For the «effective dose» of X-rays, it is usually not equal to the Gray (Gy).
| Quantity | Unit | Symbol | Derivation | Year | SI equivalent |
|---|---|---|---|---|---|
| Activity (A) | becquerel | Bq | s−1 | 1974 | SI unit |
| curie | Ci | 3.7 × 1010 s−1 | 1953 | 3.7×1010 Bq | |
| rutherford | Rd | 106 s−1 | 1946 | 1,000,000 Bq | |
| Exposure (X) | coulomb per kilogram | C/kg | C⋅kg−1 of air | 1974 | SI unit |
| röntgen | R | esu / 0.001293 g of air | 1928 | 2.58 × 10−4 C/kg | |
| Absorbed dose (D) | gray | Gy | J⋅kg−1 | 1974 | SI unit |
| erg per gram | erg/g | erg⋅g−1 | 1950 | 1.0 × 10−4 Gy | |
| rad | rad | 100 erg⋅g−1 | 1953 | 0.010 Gy | |
| Equivalent dose (H) | sievert | Sv | J⋅kg−1 × WR | 1977 | SI unit |
| röntgen equivalent man | rem | 100 erg⋅g−1 x WR | 1971 | 0.010 Sv | |
| Effective dose (E) | sievert | Sv | J⋅kg−1 × WR × WT | 1977 | SI unit |
| röntgen equivalent man | rem | 100 erg⋅g−1 × WR × WT | 1971 | 0.010 Sv |
See also[edit]
References[edit]
- ^ «X-Rays». Science Mission Directorate. NASA.
- ^ Novelline, Robert (1997). Squire’s Fundamentals of Radiology. Harvard University Press. 5th edition. ISBN 0-674-83339-2.
- ^ «X-ray». Oxford English Dictionary (Online ed.). Oxford University Press. (Subscription or participating institution membership required.)
- ^ Filler A (2009). «The History, Development and Impact of Computed Imaging in Neurological Diagnosis and Neurosurgery: CT, MRI, and DTI». Nature Precedings. doi:10.1038/npre.2009.3267.5.
- ^ Morgan W (1785-02-24). «Electrical Experiments Made in Order to Ascertain the Non-Conducting Power of a Perfect Vacuum, &c». Philosophical Transactions of the Royal Society. Royal Society of London. 75: 272–278. doi:10.1098/rstl.1785.0014.
- ^ Anderson JG (January 1945). «William Morgan and X-rays». Transactions of the Faculty of Actuaries. 17: 219–221. doi:10.1017/s0071368600003001.
- ^ Wyman T (Spring 2005). «Fernando Sanford and the Discovery of X-rays». «Imprint», from the Associates of the Stanford University Libraries: 5–15.
- ^ Thomson JJ (1903). The Discharge of Electricity through Gasses. USA: Charles Scribner’s Sons. pp. 182–186.
- ^ Mayba II, Gaida R, Kyle RA, Shampo MA (July 1997). «Ukrainian physicist contributes to the discovery of X-rays». Mayo Clinic Proceedings. Mayo Foundation for Medical Education and Research. 72 (7): 658. doi:10.1016/s0025-6196(11)63573-8. PMID 9212769. Archived from the original on 2008-05-28. Retrieved 2008-04-06.
- ^ Wiedmann’s Annalen, Vol. XLVIII.
- ^ a b Hrabak M, Padovan RS, Kralik M, Ozretic D, Potocki K (July 2008). «Scenes from the past: Nikola Tesla and the discovery of X-rays». Radiographics. 28 (4): 1189–1192. doi:10.1148/rg.284075206. PMID 18635636.
- ^ Chadda PK (2009). Hydroenergy and Its Energy Potential. Pinnacle Technology. p. 88. ISBN 978-1-61820-149-2.
- ^ Tesla’s technical publications indicate that he invented and developed a single-electrode X-ray tube. Morton, William James and Hammer, Edwin W. (1896) American Technical Book Co., p. 68. U.S. Patent 514,170, «Incandescent Electric Light». U.S. Patent 454,622 «System of Electric Lighting». These differed from other X-ray tubes in having no target electrode and worked with the output of a Tesla coil.
- ^ Stanton A (1896-01-23). «Wilhelm Conrad Röntgen On a New Kind of Rays: translation of a paper read before the Würzburg Physical and Medical Society, 1895». Nature. 53 (1369): 274–6. Bibcode:1896Natur..53R.274.. doi:10.1038/053274b0. see also pp. 268 and 276 of the same issue.
- ^ Garcia, J.; Buchwald, N. A.; Feder, B. H.; Koelling, R. A.; Tedrow, L. (1964). «Sensitivity of the head to X-ray». Science. 144 (3625): 1470–1472. doi:10.1126/science.144.3625.1470. ISSN 0036-8075. PMID 14171545. S2CID 44719943.
Rats have been trained to respond to signals consisting of very low doses of chi-ray directed to the head.
- ^ Baganha, M. F.; Marques, M. A.; Botelho, M. F.; Teixeira, M. L.; Carvalheira, V.; Calisto, J.; Silva, A.; Fernandes, A.; Torres, M.; Brito, J. (1993). «Tomodensitometry and radioisotopic methods in the study of unilateral lung hyperlucencies of vascular origin». Acta Médica Portuguesa. 6 (1): 19–24. ISSN 0870-399X. PMID 8475784.
- ^ Takahashi, K.; Case, B. W.; Dufresne, A.; Fraser, R.; Higashi, T.; Siemiatycki, J. (1994). «Relation between lung asbestos fibre burden and exposure indices based on job history». Occupational and Environmental Medicine. 51 (7): 461–469. doi:10.1136/oem.51.7.461. ISSN 1351-0711. PMC 1128015. PMID 8044245.
- ^ Karlsson EB (9 February 2000). «The Nobel Prizes in Physics 1901–2000». Stockholm: The Nobel Foundation. Retrieved 24 November 2011.
- ^ Peters P (1995). «W. C. Roentgen and the discovery of x-rays». Textbook of Radiology. Medcyclopedia.com, GE Healthcare. Archived from the original on 11 May 2008. Retrieved 5 May 2008.
- ^ Glasser O (1993). Wilhelm Conrad Röntgen and the early history of the roentgen rays. Norman Publishing. pp. 10–15. ISBN 978-0930405229.
- ^ Arthur C (2010-11-08). «Google doodle celebrates 115 years of X-rays». The Guardian. Guardian US. Retrieved 5 February 2019.
- ^ Kevles BH (1996). Naked to the Bone Medical Imaging in the Twentieth Century. Camden, NJ: Rutgers University Press. pp. 19–22. ISBN 978-0-8135-2358-3.
- ^ Sample S (2007-03-27). «X-Rays». The Electromagnetic Spectrum. NASA. Retrieved 2007-12-03.
- ^ Markel H (20 December 2012). «‘I Have Seen My Death’: How the World Discovered the X-Ray». PBS NewsHour. PBS. Retrieved 23 March 2019.
- ^ Glasser O (1958). Dr. W. C. Ro ̈ntgen. Springfield: Thomas.
- ^ Natale S (2011-11-01). «The Invisible Made Visible». Media History. 17 (4): 345–358. doi:10.1080/13688804.2011.602856. hdl:2134/19408. S2CID 142518799.
- ^ Natale S (2011-08-04). «A Cosmology of Invisible Fluids: Wireless, X-Rays, and Psychical Research Around 1900». Canadian Journal of Communication. 36 (2): 263–276. doi:10.22230/cjc.2011v36n2a2368.
- ^ Grove AW (1997-01-01). «Röntgen’s ghosts: photography, X-rays, and the Victorian imagination». Literature and Medicine. 16 (2): 141–173. doi:10.1353/lm.1997.0016. PMID 9368224. S2CID 35604474.
- ^ a b c d e f Feldman A (November 1989). «A sketch of the technical history of radiology from 1896 to 1920». Radiographics. 9 (6): 1113–1128. doi:10.1148/radiographics.9.6.2685937. PMID 2685937.
- ^ «Major John Hall-Edwards». Birmingham City Council. Archived from the original on September 28, 2012. Retrieved 2012-05-17.
- ^ Kudriashov, Y. B. (2008). Radiation Biophysics. Nova Publishers. p. xxi. ISBN 9781600212802.
- ^ «Green, James (Zoological Artist), Sciagraphs of British batrachians and reptiles, 1897». Yale Centre for British Art. Retrieved 24 November 2021.
- ^ «Sciagraphs of British Batrachians and Reptiles1». Nature. 55 (1432): 539–540. 1 April 1897. Bibcode:1897Natur..55..539.. doi:10.1038/055539a0. S2CID 4054184.
- ^ a b Spiegel PK (January 1995). «The first clinical X-ray made in America—100 years». AJR. American Journal of Roentgenology. 164 (1): 241–243. doi:10.2214/ajr.164.1.7998549. PMID 7998549.
- ^ Nicolaas A. Rupke, Eminent Lives in Twentieth-Century Science and Religion, page 300, Peter Lang, 2009 ISBN 3631581203
- ^ «Visible Proofs: Forensic Views of the Body: Galleries: Cases: Could X-rays Have Saved President William McKinley?». www.nlm.nih.gov. Retrieved 2022-01-24.
- ^ Daniel J (April 1896). «THE X-RAYS». Science. 3 (67): 562–563. Bibcode:1896Sci…..3..562D. doi:10.1126/science.3.67.562. PMID 17779817.
- ^ Fleming WL (1909). The South in the Building of the Nation: Biography A-J. Pelican Publishing. p. 300. ISBN 978-1589809468.
- ^ Ce4Rt (Mar 2014). Understanding Ionizing Radiation and Protection. p. 174.
- ^ Glasser O (1934). Wilhelm Conrad Röntgen and the Early History of the Roentgen Rays. Norman Publishing. p. 294. ISBN 978-0930405229.
- ^ Sansare K, Khanna V, Karjodkar F (February 2011). «Early victims of X-rays: a tribute and current perception». Dento Maxillo Facial Radiology. 40 (2): 123–125. doi:10.1259/dmfr/73488299. PMC 3520298. PMID 21239576.
- ^ a b «ISU Health Physics Radinf — First 50 Years». sites.google.com. Retrieved 2022-01-24.
- ^ California, San Francisco Area Funeral Home Records, 1835–1979. Database with images. FamilySearch. Jacob Fleischman in the entry for Elizabeth Aschheim. 03 Aug 1905. Citing funeral home J.S. Godeau, San Francisco, San Francisco, California. Record book Vol. 06, p. 1–400, 1904–1906. San Francisco Public Library. San Francisco History and Archive Center.
- ^ Editor. (August 5, 1905). Aschheim. Obituaries. San Francisco Examiner. San Francisco, California.
- ^ Editor. (August 5, 1905). Obituary Notice. Elizabeth Fleischmann. San Francisco Chronicle. Page 10.
- ^ «Major John Hall-Edwards». Birmingham City Council. Archived from the original on 28 September 2012. Retrieved 23 April 2010.
- ^ a b Schall K (1905). Electro-medical Instruments and their Management. Bemrose & Sons Ltd. Printers. pp. 96, 107.
- ^ Stoddart C (1 March 2022). «Structural biology: How proteins got their close-up». Knowable Magazine. doi:10.1146/knowable-022822-1. Retrieved 25 March 2022.
- ^ Birmingham City Council: Major John Hall-Edwards Archived September 28, 2012, at the Wayback Machine
- ^ «X-ray movies show hard boiled egg fighting digestive organs (1913)». The News-Palladium. 1913-04-04. p. 2. Retrieved 2020-11-26.
- ^ «X-ray moving pictures latest (1913)». Chicago Tribune. 1913-06-22. p. 32. Retrieved 2020-11-26.
- ^ «Homeopaths to show movies of body’s organs at work (1915)». The Central New Jersey Home News. 1915-05-10. p. 6. Retrieved 2020-11-26.
- ^ «How X-Ray Movies Are Taken (1918)». Davis County Clipper. 1918-03-15. p. 2. Retrieved 2020-11-26.
- ^ «X-ray movies (1919)». Tampa Bay Times. 1919-01-12. p. 16. Retrieved 2020-11-26.
- ^ «X-ray movies perfected. Will show motions of bones and joints of human body. (1918)». The Sun. 1918-01-07. p. 7. Retrieved 2020-11-26.
- ^ «Talk is cheap? X-ray used by Institute of Phonetics (1920)». New Castle Herald. 1920-01-02. p. 13. Retrieved 2020-11-26.
- ^ Jorgensen TJ (10 October 2017). «Marie Curie and her X-ray vehicles’ contribution to World War I battlefield medicine». The Conversation. Retrieved February 23, 2018.
- ^ «X-Rays for Fitting Boots». Warwick Daily News (Qld.: 1919–1954). 1921-08-25. p. 4. Retrieved 2020-11-27.
- ^ «T. C. BEIRNE’S X-RAY SHOE FITTING». Telegraph (Brisbane, Qld. : 1872–1947). 1925-07-17. p. 8. Retrieved 2017-11-05.
- ^ «THE PEDOSCOPE». Sunday Times (Perth, WA : 1902–1954). 1928-07-15. p. 5. Retrieved 2017-11-05.
- ^ «X-RAY SHOE FITTINGS». Biz (Fairfield, NSW : 1928–1972). 1955-07-27. p. 10. Retrieved 2017-11-05.
- ^ «SHOE X-RAY DANGERS». Brisbane Telegraph (Qld. : 1948–1954). 1951-02-28. p. 7. Retrieved 2017-11-05.
- ^ «X-ray shoe sets in S.A. ‘controlled’«. News (Adelaide, SA : 1923–1954). 1951-04-27. p. 12. Retrieved 2017-11-05.
- ^ «Ban On Shoe X-ray Machines Resented». Canberra Times (ACT : 1926–1995). 1957-06-26. p. 4. Retrieved 2017-11-05.
- ^ Fitzgerald R (2000). «Phase-sensitive x-ray imaging». Physics Today. 53 (7): 23–26. Bibcode:2000PhT….53g..23F. doi:10.1063/1.1292471. S2CID 121322301.
- ^ a b David C, Nöhammer B, Solak H, Ziegler (2002). «Differential x-ray phase contrast imaging using a shearing interferometer». Applied Physics Letters. 81 (17): 3287–3289. Bibcode:2002ApPhL..81.3287D. doi:10.1063/1.1516611.
- ^ Wilkins SW, Gureyev TE, Gao D, Pogany A, Stevenson AW (1996). «Phase-contrast imaging using polychromatic hard X-rays». Nature. 384 (6607): 335–338. Bibcode:1996Natur.384..335W. doi:10.1038/384335a0. S2CID 4273199.
- ^ Davis TJ, Gao D, Gureyev TE, Stevenson AW, Wilkins SW (1995). «Phase-contrast imaging of weakly absorbing materials using hard X-rays». Nature. 373 (6515): 595–598. Bibcode:1995Natur.373..595D. doi:10.1038/373595a0. S2CID 4287341.
- ^ Momose A, Takeda T, Itai Y, Hirano K (April 1996). «Phase-contrast X-ray computed tomography for observing biological soft tissues». Nature Medicine. 2 (4): 473–475. doi:10.1038/nm0496-473. PMID 8597962. S2CID 23523144.
- ^ Attwood, David (1999). Soft X-rays and extreme ultraviolet radiation. Cambridge University. p. 2. ISBN 978-0-521-65214-8. Archived from the original on 2012-11-11. Retrieved 2012-11-04.
- ^ «Physics.nist.gov». Physics.nist.gov. Retrieved 2011-11-08.
- ^ a b Denny PP, Heaton B (1999). Physics for Diagnostic Radiology. USA: CRC Press. p. 12. ISBN 978-0-7503-0591-4.
- ^ Feynman R, Leighton R, Sands M (1963). The Feynman Lectures on Physics. Vol. 1. USA: Addison-Wesley. pp. 2–5. ISBN 978-0-201-02116-5.
- ^ L’Annunziata M, Abrade M (2003). Handbook of Radioactivity Analysis. Academic Press. p. 58. ISBN 978-0-12-436603-9.
- ^ Grupen C, Cowan G, Eidelman SD, Stroh T (2005). Astroparticle Physics. Springer. p. 109. ISBN 978-3-540-25312-9.
- ^ Hodgman, Charles, ed. (1961). CRC Handbook of Chemistry and Physics, 44th Ed. USA: Chemical Rubber Co. p. 2850.
- ^ Government of Canada, Canadian Centre for Occupational Health and Safety (2019-05-09). «Radiation – Quantities and Units of Ionizing Radiation: OSH Answers». www.ccohs.ca. Retrieved 2019-05-09.
- ^ Bushberg, Jerrold T.; Seibert, J. Anthony; Leidholdt, Edwin M.; Boone, John M. (2002). The essential physics of medical imaging. Lippincott Williams & Wilkins. p. 42. ISBN 978-0-683-30118-2.
- ^ Bushberg, Jerrold T.; Seibert, J. Anthony; Leidholdt, Edwin M.; Boone, John M. (2002). The essential physics of medical imaging. Lippincott Williams & Wilkins. p. 38. ISBN 978-0-683-30118-2.
- ^ Kissel L (2000-09-02). «RTAB: the Rayleigh scattering database». Radiation Physics and Chemistry. Lynn Kissel. 59 (2): 185–200. Bibcode:2000RaPC…59..185K. doi:10.1016/S0969-806X(00)00290-5. Archived from the original on 2011-12-12. Retrieved 2012-11-08.
- ^ Attwood, David (1999). «3». Soft X-rays and extreme ultraviolet radiation. Cambridge University Press. ISBN 978-0-521-65214-8. Archived from the original on 2012-11-11. Retrieved 2012-11-04.
- ^ «X-ray Transition Energies Database». NIST Physical Measurement Laboratory. 2011-12-09. Retrieved 2016-02-19.
- ^ «X-Ray Data Booklet Table 1-3» (PDF). Center for X-ray Optics and Advanced Light Source, Lawrence Berkeley National Laboratory. 2009-10-01. Archived from the original (PDF) on 23 April 2009. Retrieved 2016-02-19.
- ^ Whaites E, Cawson R (2002). Essentials of Dental Radiography and Radiology. Elsevier Health Sciences. pp. 15–20. ISBN 978-0-443-07027-3.
- ^ Bushburg J, Seibert A, Leidholdt E, Boone J (2002). The Essential Physics of Medical Imaging. USA: Lippincott Williams & Wilkins. p. 116. ISBN 978-0-683-30118-2.
- ^ Emilio B, Ballerna A (1994). «Preface». Biomedical Applications of Synchrotron Radiation: Proceedings of the 128th Course at the International School of Physics -Enrico Fermi- 12–22 July 1994, Varenna, Italy. IOS Press. p. xv. ISBN 90-5199-248-3.
- ^ Camara CG, Escobar JV, Hird JR, Putterman SJ (2008). «Correlation between nanosecond X-ray flashes and stick–slip friction in peeling tape» (PDF). Nature. 455 (7216): 1089–1092. Bibcode:2008Natur.455.1089C. doi:10.1038/nature07378. S2CID 4372536. Retrieved 2 February 2013.
- ^ Paul H, Muhr J (1986). «Review of experimental cross sections for K-shell ionization by light ions». Physics Reports. 135 (2): 47–97. Bibcode:1986PhR…135…47P. doi:10.1016/0370-1573(86)90149-3.
- ^ Köhn C, Ebert U (2014). «Angular distribution of Bremsstrahlung photons and of positrons for calculations of terrestrial gamma-ray flashes and positron beams». Atmospheric Research. 135–136: 432–465. arXiv:1202.4879. Bibcode:2014AtmRe.135..432K. doi:10.1016/j.atmosres.2013.03.012. S2CID 10679475.
- ^ Köhn C, Ebert U (2015). «Calculation of beams of positrons, neutrons, and protons associated with terrestrial gamma ray flashes». Journal of Geophysical Research: Atmospheres. 120 (4): 1620–1635. Bibcode:2015JGRD..120.1620K. doi:10.1002/2014JD022229.
- ^ Kochkin P, Köhn C, Ebert U, Van Deursen L (May 2016). «Analyzing x-ray emissions from meter-scale negative discharges in ambient air». Plasma Sources Science and Technology. 25 (4): 044002. Bibcode:2016PSST…25d4002K. doi:10.1088/0963-0252/25/4/044002. S2CID 43609721.
- ^ Cooray V, Arevalo L, Rahman M, Dwyer J, Rassoul H (2009). «On the possible origin of X-rays in long laboratory sparks». Journal of Atmospheric and Solar-Terrestrial Physics. 71 (17–18): 1890–1898. Bibcode:2009JASTP..71.1890C. doi:10.1016/j.jastp.2009.07.010.
- ^ Köhn C, Chanrion O, Neubert T (March 2017). «Electron acceleration during streamer collisions in air». Geophysical Research Letters. 44 (5): 2604–2613. Bibcode:2017GeoRL..44.2604K. doi:10.1002/2016GL072216. PMC 5405581. PMID 28503005.
- ^ Köhn C, Chanrion O, Babich LP, Neubert T (2018). «Streamer properties and associated x-rays in perturbed air». Plasma Sources Science and Technology. 27 (1): 015017. Bibcode:2018PSST…27a5017K. doi:10.1088/1361-6595/aaa5d8.
- ^ Köhn C, Chanrion O, Neubert T (May 2018). «High-Energy Emissions Induced by Air Density Fluctuations of Discharges». Geophysical Research Letters. 45 (10): 5194–5203. Bibcode:2018GeoRL..45.5194K. doi:10.1029/2018GL077788. PMC 6049893. PMID 30034044.
- ^ Förster A, Brandstetter S, Schulze-Briese C (June 2019). «Transforming X-ray detection with hybrid photon counting detectors». Philosophical Transactions. Series A, Mathematical, Physical, and Engineering Sciences. 377 (2147): 20180241. Bibcode:2019RSPTA.37780241F. doi:10.1098/rsta.2018.0241. PMC 6501887. PMID 31030653.
- ^ «Roentgen’s discovery of the x-ray». www.bl.uk. Retrieved 2019-05-09.
- ^ a b Roobottom CA, Mitchell G, Morgan-Hughes G (November 2010). «Radiation-reduction strategies in cardiac computed tomographic angiography». Clinical Radiology. 65 (11): 859–867. doi:10.1016/j.crad.2010.04.021. PMID 20933639.
Of the 5 billion imaging investigations performed worldwide…
- ^ a b «Medical Radiation Exposure Of The U.S. Population Greatly Increased Since The Early 1980s». ScienceDaily. Retrieved 2022-01-24.
- ^ Van Haver A, Kolk S, DeBoodt S, Valkering K, Verdonk P (2018). «Accuracy of total knee implant position assessment based on postoperative X-rays, registered to pre-operative CT-based 3D models». Orthopaedic Proceedings. 99-B (Supp 4).
- ^ Herman GT (2009). Fundamentals of Computerized Tomography: Image Reconstruction from Projections (2nd ed.). Springer. ISBN 978-1-85233-617-2.
- ^ Advances in kilovoltage x-ray beam dosimetry in Hill R, Healy B, Holloway L, Kuncic Z, Thwaites D, Baldock C (March 2014). «Advances in kilovoltage x-ray beam dosimetry». Physics in Medicine and Biology. 59 (6): R183–R231. Bibcode:2014PMB….59R.183H. doi:10.1088/0031-9155/59/6/r183. PMID 24584183. S2CID 18082594.
- ^ Thwaites DI, Tuohy JB (July 2006). «Back to the future: the history and development of the clinical linear accelerator». Physics in Medicine and Biology. 51 (13): R343–R362. Bibcode:2006PMB….51R.343T. doi:10.1088/0031-9155/51/13/R20. PMID 16790912. S2CID 7672187.
- ^ Hall EJ, Brenner DJ (May 2008). «Cancer risks from diagnostic radiology». The British Journal of Radiology. 81 (965): 362–378. doi:10.1259/bjr/01948454. PMID 18440940.
- ^ Brenner DJ (2010). «Should we be concerned about the rapid increase in CT usage?». Reviews on Environmental Health. 25 (1): 63–68. doi:10.1515/REVEH.2010.25.1.63. PMID 20429161. S2CID 17264651.
- ^ De Santis M, Cesari E, Nobili E, Straface G, Cavaliere AF, Caruso A (September 2007). «Radiation effects on development». Birth Defects Research. Part C, Embryo Today. 81 (3): 177–182. doi:10.1002/bdrc.20099. PMID 17963274.
- ^ «11th Report on Carcinogens». Ntp.niehs.nih.gov. Archived from the original on 2010-12-09. Retrieved 2010-11-08.
- ^ a b c Brenner DJ, Hall EJ (November 2007). «Computed tomography—an increasing source of radiation exposure». The New England Journal of Medicine. 357 (22): 2277–2284. doi:10.1056/NEJMra072149. PMID 18046031. S2CID 2760372.
- ^ Upton AC (July 2003). «The state of the art in the 1990’s: NCRP Report No. 136 on the scientific bases for linearity in the dose-response relationship for ionizing radiation». Health Physics. 85 (1): 15–22. doi:10.1097/00004032-200307000-00005. PMID 12852466. S2CID 13301920.
- ^ Calabrese EJ, Baldwin LA (February 2003). «Toxicology rethinks its central belief» (PDF). Nature. 421 (6924): 691–692. Bibcode:2003Natur.421..691C. doi:10.1038/421691a. PMID 12610596. S2CID 4419048. Archived from the original (PDF) on 2011-09-12.
- ^ Oakley PA, Ehsani NN, Harrison DE (2019-04-01). «The Scoliosis Quandary: Are Radiation Exposures From Repeated X-Rays Harmful?». Dose-Response. 17 (2): 1559325819852810. doi:10.1177/1559325819852810. PMC 6560808. PMID 31217755.
- ^ Berrington de González A, Darby S (January 2004). «Risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries». Lancet. 363 (9406): 345–351. doi:10.1016/S0140-6736(04)15433-0. PMID 15070562. S2CID 8516754.
- ^ a b Radiology (ACR), Radiological Society of North America (RSNA) and American College of. «Radiation Dose in X-Ray and CT Exams». Radiologyinfo.org. Retrieved 2022-01-24.
- ^ «National Cancer Institute: Surveillance Epidemiology and End Results (SEER) data». Seer.cancer.gov. 2010-06-30. Retrieved 2011-11-08.
- ^ Caon M, Bibbo G, Pattison J (2000). «Monte Carlo calculated effective dose to teenage girls from computed tomography examinations». Radiation Protection Dosimetry. 90 (4): 445–448. doi:10.1093/oxfordjournals.rpd.a033172.
- ^ Shrimpton, P.C; Miller, H.C; Lewis, M.A; Dunn, M. Doses from Computed Tomography (CT) examinations in the UK – 2003 Review Archived September 22, 2011, at the Wayback Machine
- ^ Gregory KJ, Bibbo G, Pattison JE (August 2008). «On the uncertainties in effective dose estimates of adult CT head scans». Medical Physics. 35 (8): 3501–3510. Bibcode:2008MedPh..35.3501G. doi:10.1118/1.2952359. PMID 18777910.
- ^ Giles D, Hewitt D, Stewart A, Webb J (September 1956). «Malignant disease in childhood and diagnostic irradiation in utero». Lancet. 271 (6940): 447. doi:10.1016/S0140-6736(56)91923-7. PMID 13358242.
- ^ «Pregnant Women and Radiation Exposure». eMedicine Live online medical consultation. Medscape. 28 December 2008. Archived from the original on January 23, 2009. Retrieved 2009-01-16.
- ^ a b c Ratnapalan S, Bentur Y, Koren G (December 2008). ««Doctor, will that x-ray harm my unborn child?»«. CMAJ. 179 (12): 1293–1296. doi:10.1503/cmaj.080247. PMC 2585137. PMID 19047611.
- ^ Donnelly LF (February 2005). «Reducing radiation dose associated with pediatric CT by decreasing unnecessary examinations». AJR. American Journal of Roentgenology. 184 (2): 655–657. doi:10.2214/ajr.184.2.01840655. PMID 15671393.
- ^ US National Research Council (2006). Health Risks from Low Levels of Ionizing Radiation, BEIR 7 phase 2. National Academies Press. pp. 5, fig.PS–2. ISBN 978-0-309-09156-5., data credited to NCRP (US National Committee on Radiation Protection) 1987
- ^ «ANS / Public Information / Resources / Radiation Dose Calculator». Archived from the original on 2012-05-16. Retrieved 2012-05-16.
- ^ «HOW DANGEROUS IS RADIATION?». www.phyast.pitt.edu. Retrieved 2022-01-24.
- ^ Muller, Richard. Physics for Future Presidents, Princeton University Press, 2010
- ^ X-Rays Archived 2007-03-15 at the Wayback Machine. Doctorspiller.com (2007-05-09). Retrieved on 2011-05-05.
- ^ X-Ray Safety Archived April 4, 2007, at the Wayback Machine. Dentalgentlecare.com (2008-02-06). Retrieved on 2011-05-05.
- ^ «Dental X-Rays». Idaho State University. Retrieved November 7, 2012.
- ^ D.O.E. – About Radiation Archived April 27, 2012, at the Wayback Machine
- ^ Chalkley M, Listl S (March 2018). «First do no harm — The impact of financial incentives on dental X-rays». Journal of Health Economics. 58 (March 2018): 1–9. doi:10.1016/j.jhealeco.2017.12.005. PMID 29408150.
- ^ «Using lasers instead of x-rays». Open University. 24 February 2011. Retrieved 28 July 2021.
- ^ Dent S (12 February 2015). «Scientists achieve X-ray vision with safe, visible light». Engadget. Retrieved 28 July 2021.
- ^ Kasai N, Kakudo, M (2005). X-ray diffraction by macromolecules. Tokyo: Kodansha. pp. 291–2. ISBN 978-3-540-25317-4.
- ^ Monico L, Van der Snickt G, Janssens K, De Nolf W, Miliani C, Verbeeck J, et al. (February 2011). «Degradation process of lead chromate in paintings by Vincent van Gogh studied by means of synchrotron X-ray spectromicroscopy and related methods. 1. Artificially aged model samples». Analytical Chemistry. 83 (4): 1214–1223. doi:10.1021/ac102424h. PMID 21314201. Monico L, Van der Snickt G, Janssens K, De Nolf W, Miliani C, Dik J, et al. (February 2011). «Degradation process of lead chromate in paintings by Vincent van Gogh studied by means of synchrotron X-ray spectromicroscopy and related methods. 2. Original paint layer samples». Analytical Chemistry. 83 (4): 1224–1231. doi:10.1021/ac1025122. PMID 21314202.
- ^ Ahi K, Anwar M (May 2016). «Advanced terahertz techniques for quality control and counterfeit detection». In Anwar MF, Crowe TW, Manzur T (eds.). Terahertz Physics, Devices, and Systems X: Advanced Applications in Industry and Defense. Vol. 9856. Society of Photographic Instrumentation Engineers. pp. 31–44.
- ^ Bickmore, Helen (2003). Milady’s Hair Removal Techniques: A Comprehensive Manual. ISBN 978-1401815554.
- ^ Frame P. «Wilhelm Röntgen and the Invisible Light». Tales from the Atomic Age. Oak Ridge Associated Universities. Retrieved 2021-10-11.
- ^ European Synchrotron Radiation Facility ID11
- ^ Als-Nielsen, Jens; Mcmorrow, Des (2001). Elements of Modern X-Ray Physics. John Wiley & Sons Ltd. pp. 40–41. ISBN 978-0-471-49858-2.
External links[edit]
- «On a New Kind of Rays». Nature. 53 (1369): 274–276. January 1896. Bibcode:1896Natur..53R.274.. doi:10.1038/053274b0.
- «Ion X-Ray tubes». The Cathode Ray Tube site.
- «Index of Early Bremsstrahlung Articles». Shade Tree Physics. 12 April 2010.
- Samuel JJ (20 October 2013). «La découverte des rayons X par Röntgen». Bibnum Education (in French). Röntgen’s discovery of X-rays (PDF; English translation)
- Oakley, P. A., Navid Ehsani, N., & Harrison, D. E. (2020). 5 Reasons Why Scoliosis X-Rays Are Not Harmful. Dose-Response. https://doi.org/10.1177/1559325820957797
This article is about the nature, production, and uses of the radiation. For the method of imaging, see Radiography. For the medical specialty, see Radiology. For other uses, see X-ray (disambiguation). Not to be confused with X-wave or X-band.
Natural color X-ray photogram of a wine scene. Note the edges of hollow cylinders as compared to the solid candle.
An X-ray, or, much less commonly, X-radiation, is a penetrating form of high-energy electromagnetic radiation. Most X-rays have a wavelength ranging from 10 picometers to 10 nanometers, corresponding to frequencies in the range 30 petahertz to 30 exahertz (3×1016 Hz to 3×1019 Hz) and energies in the range 145 eV to 124 keV. X-ray wavelengths are shorter than those of UV rays and typically longer than those of gamma rays. In many languages, X-radiation is referred to as Röntgen radiation, after the German scientist Wilhelm Conrad Röntgen, who discovered it on November 8, 1895.[1] He named it X-radiation to signify an unknown type of radiation.[2] Spellings of X-ray(s) in English include the variants x-ray(s), xray(s), and X ray(s).[3] The most familiar use of X-rays is checking for fractures (broken bones), but X-rays are also used in other ways. For example, chest X-rays can spot pneumonia. Mammograms use X-rays to look for breast cancer.
History[edit]
Pre-Röntgen observations and research[edit]
Before their discovery in 1895, X-rays were just a type of unidentified radiation emanating from experimental discharge tubes. They were noticed by scientists investigating cathode rays produced by such tubes, which are energetic electron beams that were first observed in 1869. Many of the early Crookes tubes (invented around 1875) undoubtedly radiated X-rays, because early researchers noticed effects that were attributable to them, as detailed below. Crookes tubes created free electrons by ionization of the residual air in the tube by a high DC voltage of anywhere between a few kilovolts and 100 kV. This voltage accelerated the electrons coming from the cathode to a high enough velocity that they created X-rays when they struck the anode or the glass wall of the tube.[4]
The earliest experimenter thought to have (unknowingly) produced X-rays was William Morgan. In 1785, he presented a paper to the Royal Society of London describing the effects of passing electrical currents through a partially evacuated glass tube, producing a glow created by X-rays.[5][6] This work was further explored by Humphry Davy and his assistant Michael Faraday.
When Stanford University physics professor Fernando Sanford created his «electric photography», he also unknowingly generated and detected X-rays. From 1886 to 1888, he had studied in the Hermann von Helmholtz laboratory in Berlin, where he became familiar with the cathode rays generated in vacuum tubes when a voltage was applied across separate electrodes, as previously studied by Heinrich Hertz and Philipp Lenard. His letter of January 6, 1893 (describing his discovery as «electric photography») to the Physical Review was duly published and an article entitled Without Lens or Light, Photographs Taken With Plate and Object in Darkness appeared in the San Francisco Examiner.[7]
Starting in 1888, Philipp Lenard conducted experiments to see whether cathode rays could pass out of the Crookes tube into the air. He built a Crookes tube with a «window» at the end made of thin aluminium, facing the cathode so the cathode rays would strike it (later called a «Lenard tube»). He found that something came through, that would expose photographic plates and cause fluorescence. He measured the penetrating power of these rays through various materials. It has been suggested that at least some of these «Lenard rays» were actually X-rays.[8]
In 1889, Ukrainian-born Ivan Puluj, a lecturer in experimental physics at the Prague Polytechnic who since 1877 had been constructing various designs of gas-filled tubes to investigate their properties, published a paper on how sealed photographic plates became dark when exposed to the emanations from the tubes.[9]
Helmholtz formulated mathematical equations for X-rays. He postulated a dispersion theory before Röntgen made his discovery and announcement. He based it on the electromagnetic theory of light.[10][full citation needed] However, he did not work with actual X-rays.
In 1894, Nikola Tesla noticed damaged film in his lab that seemed to be associated with Crookes tube experiments and began investigating this invisible, radiant energy.[11][12] After Röntgen identified the X-ray, Tesla began making X-ray images of his own using high voltages and tubes of his own design,[13] as well as Crookes tubes.
Discovery by Röntgen[edit]
On November 8, 1895, German physics professor Wilhelm Röntgen stumbled on X-rays while experimenting with Lenard tubes and Crookes tubes and began studying them. He wrote an initial report «On a new kind of ray: A preliminary communication» and on December 28, 1895, submitted it to Würzburg’s Physical-Medical Society journal.[14] This was the first paper written on X-rays. Röntgen referred to the radiation as «X», to indicate that it was an unknown type of radiation. Some early texts refer to them as Chi-rays having interpreted «X» as the uppercase Greek letter Chi, Χ.[15][16][17] The name X-rays stuck, although (over Röntgen’s great objections) many of his colleagues suggested calling them Röntgen rays. They are still referred to as such in many languages, including German, Hungarian, Ukrainian, Danish, Polish, Czech, Bulgarian, Swedish, Finnish, Estonian, Slovenian, Turkish, Russian, Latvian, Lithuanian, Albanian, Japanese, Dutch, Georgian, Hebrew, and Norwegian. Röntgen received the first Nobel Prize in Physics for his discovery.[18]
There are conflicting accounts of his discovery because Röntgen had his lab notes burned after his death, but this is a likely reconstruction by his biographers:[19][20] Röntgen was investigating cathode rays from a Crookes tube which he had wrapped in black cardboard so that the visible light from the tube would not interfere, using a fluorescent screen painted with barium platinocyanide. He noticed a faint green glow from the screen, about 1 meter (3.3 ft) away. Röntgen realized some invisible rays coming from the tube were passing through the cardboard to make the screen glow. He found they could also pass through books and papers on his desk. Röntgen threw himself into investigating these unknown rays systematically. Two months after his initial discovery, he published his paper.[21]
Röntgen discovered their medical use when he made a picture of his wife’s hand on a photographic plate formed due to X-rays. The photograph of his wife’s hand was the first photograph of a human body part using X-rays. When she saw the picture, she said «I have seen my death.»[24]
The discovery of X-rays stimulated a veritable sensation. Röntgen’s biographer Otto Glasser estimated that, in 1896 alone, as many as 49 essays and 1044 articles about the new rays were published.[25] This was probably a conservative estimate, if one considers that nearly every paper around the world extensively reported about the new discovery, with a magazine such as Science dedicating as many as 23 articles to it in that year alone.[26] Sensationalist reactions to the new discovery included publications linking the new kind of rays to occult and paranormal theories, such as telepathy.[27][28]
Advances in radiology[edit]
Taking an X-ray image with early Crookes tube apparatus, late 1800s. The Crookes tube is visible in center. The standing man is viewing his hand with a fluoroscope screen. The seated man is taking a radiograph of his hand by placing it on a photographic plate. No precautions against radiation exposure are taken; its hazards were not known at the time.
Surgical removal of a bullet whose location was diagnosed with X-rays (see inset) in 1897
Röntgen immediately noticed X-rays could have medical applications. Along with his 28 December Physical-Medical Society submission, he sent a letter to physicians he knew around Europe (January 1, 1896).[29] News (and the creation of «shadowgrams») spread rapidly with Scottish electrical engineer Alan Archibald Campbell-Swinton being the first after Röntgen to create an X-ray (of a hand). Through February, there were 46 experimenters taking up the technique in North America alone.[29]
The first use of X-rays under clinical conditions was by John Hall-Edwards in Birmingham, England on 11 January 1896, when he radiographed a needle stuck in the hand of an associate. On February 14, 1896, Hall-Edwards was also the first to use X-rays in a surgical operation.[30]
In early 1896, several weeks after Röntgen’s discovery, Ivan Romanovich Tarkhanov irradiated frogs and insects with X-rays, concluding that the rays «not only photograph, but also affect the living function».[31] At around the same time, the zoological illustrator James Green began to use X-rays to examine fragile specimens. George Albert Boulenger first mentioned this work in a paper he delivered before the Zoological Society of London in May 1896. The book Sciagraphs of British Batrachians and Reptiles (sciagraph is an obsolete name for an X-ray photograph), by Green and James H. Gardiner, with a foreword by Boulenger, was published in 1897.[32][33]
The first medical X-ray made in the United States was obtained using a discharge tube of Pului’s design. In January 1896, on reading of Röntgen’s discovery, Frank Austin of Dartmouth College tested all of the discharge tubes in the physics laboratory and found that only the Pului tube produced X-rays. This was a result of Pului’s inclusion of an oblique «target» of mica, used for holding samples of fluorescent material, within the tube. On 3 February 1896, Gilman Frost, professor of medicine at the college, and his brother Edwin Frost, professor of physics, exposed the wrist of Eddie McCarthy, whom Gilman had treated some weeks earlier for a fracture, to the X-rays and collected the resulting image of the broken bone on gelatin photographic plates obtained from Howard Langill, a local photographer also interested in Röntgen’s work.[34]
1896 plaque published in «Nouvelle Iconographie de la Salpetrière», a medical journal. In the left a hand deformity, in the right same hand seen using radiography. The authors named the technique Röntgen photography.
Many experimenters, including Röntgen himself in his original experiments, came up with methods to view X-ray images «live» using some form of luminescent screen.[29] Röntgen used a screen coated with barium platinocyanide. On February 5, 1896, live imaging devices were developed by both Italian scientist Enrico Salvioni (his «cryptoscope») and Professor McGie of Princeton University (his «Skiascope»), both using barium platinocyanide. American inventor Thomas Edison started research soon after Röntgen’s discovery and investigated materials’ ability to fluoresce when exposed to X-rays, finding that calcium tungstate was the most effective substance. In May 1896, he developed the first mass-produced live imaging device, his «Vitascope», later called the fluoroscope, which became the standard for medical X-ray examinations.[29] Edison dropped X-ray research around 1903, before the death of Clarence Madison Dally, one of his glassblowers. Dally had a habit of testing X-ray tubes on his own hands, developing a cancer in them so tenacious that both arms were amputated in a futile attempt to save his life; in 1904, he became the first known death attributed to X-ray exposure.[29] During the time the fluoroscope was being developed, Serbian American physicist Mihajlo Pupin, using a calcium tungstate screen developed by Edison, found that using a fluorescent screen decreased the exposure time it took to create an X-ray for medical imaging from an hour to a few minutes.[35][29]
In 1901, U.S. President William McKinley was shot twice in an assassination attempt while attending the Pan American Exposition in Buffalo, New York. While one bullet only grazed his sternum, another had lodged somewhere deep inside his abdomen and could not be found. A worried McKinley aide sent word to inventor Thomas Edison to rush an X-ray machine to Buffalo to find the stray bullet. It arrived but was not used. While the shooting itself had not been lethal, gangrene had developed along the path of the bullet, and McKinley died of septic shock due to bacterial infection six days later.[36]
Hazards discovered[edit]
With the widespread experimentation with X‑rays after their discovery in 1895 by scientists, physicians, and inventors came many stories of burns, hair loss, and worse in technical journals of the time. In February 1896, Professor John Daniel and Dr. William Lofland Dudley of Vanderbilt University reported hair loss after Dr. Dudley was X-rayed. A child who had been shot in the head was brought to the Vanderbilt laboratory in 1896. Before trying to find the bullet, an experiment was attempted, for which Dudley «with his characteristic devotion to science»[37][38][39] volunteered. Daniel reported that 21 days after taking a picture of Dudley’s skull (with an exposure time of one hour), he noticed a bald spot 5 centimeters (2 in) in diameter on the part of his head nearest the X-ray tube: «A plate holder with the plates towards the side of the skull was fastened and a coin placed between the skull and the head. The tube was fastened at the other side at a distance of one-half inch [1.3 cm] from the hair.»[40]
In August 1896, Dr. HD. Hawks, a graduate of Columbia College, suffered severe hand and chest burns from an X-ray demonstration. It was reported in Electrical Review and led to many other reports of problems associated with X-rays being sent in to the publication.[41] Many experimenters including Elihu Thomson at Edison’s lab, William J. Morton, and Nikola Tesla also reported burns. Elihu Thomson deliberately exposed a finger to an X-ray tube over a period of time and suffered pain, swelling, and blistering.[42] Other effects were sometimes blamed for the damage including ultraviolet rays and (according to Tesla) ozone.[11] Many physicians claimed there were no effects from X-ray exposure at all.[42] On August 3, 1905, in San Francisco, California, Elizabeth Fleischman, an American X-ray pioneer, died from complications as a result of her work with X-rays.[43][44][45]
Hall-Edwards developed a cancer (then called X-ray dermatitis) sufficiently advanced by 1904 to cause him to write papers and give public addresses on the dangers of X-rays. His left arm had to be amputated at the elbow in 1908,[46] and four fingers on his right arm soon thereafter, leaving only a thumb. He died of cancer in 1926. His left hand is kept at Birmingham University.
20th century and beyond[edit]
A patient being examined with a thoracic fluoroscope in 1940, which displayed continuous moving images. This image was used to argue that radiation exposure during the X-ray procedure would be negligible.
The many applications of X-rays immediately generated enormous interest. Workshops began making specialized versions of Crookes tubes for generating X-rays and these first-generation cold cathode or Crookes X-ray tubes were used until about 1920.
A typical early 20th century medical X-ray system consisted of a Ruhmkorff coil connected to a cold cathode Crookes X-ray tube. A spark gap was typically connected to the high voltage side in parallel to the tube and used for diagnostic purposes.[47] The spark gap allowed detecting the polarity of the sparks, measuring voltage by the length of the sparks thus determining the «hardness» of the vacuum of the tube, and it provided a load in the event the X-ray tube was disconnected. To detect the hardness of the tube, the spark gap was initially opened to the widest setting. While the coil was operating, the operator reduced the gap until sparks began to appear. A tube in which the spark gap began to spark at around 6.4 centimeters (2.5 in) was considered soft (low vacuum) and suitable for thin body parts such as hands and arms. A 13-centimeter (5 in) spark indicated the tube was suitable for shoulders and knees. An 18-to-23-centimeter (7 to 9 in) spark would indicate a higher vacuum suitable for imaging the abdomen of larger individuals. Since the spark gap was connected in parallel to the tube, the spark gap had to be opened until the sparking ceased in order to operate the tube for imaging. Exposure time for photographic plates was around half a minute for a hand to a couple of minutes for a thorax. The plates may have a small addition of fluorescent salt to reduce exposure times.[47]
Crookes tubes were unreliable. They had to contain a small quantity of gas (invariably air) as a current will not flow in such a tube if they are fully evacuated. However, as time passed, the X-rays caused the glass to absorb the gas, causing the tube to generate «harder» X-rays until it soon stopped operating. Larger and more frequently used tubes were provided with devices for restoring the air, known as «softeners». These often took the form of a small side tube that contained a small piece of mica, a mineral that traps relatively large quantities of air within its structure. A small electrical heater heated the mica, causing it to release a small amount of air, thus restoring the tube’s efficiency. However, the mica had a limited life, and the restoration process was difficult to control.
In 1904, John Ambrose Fleming invented the thermionic diode, the first kind of vacuum tube. This used a hot cathode that caused an electric current to flow in a vacuum. This idea was quickly applied to X-ray tubes, and hence heated-cathode X-ray tubes, called «Coolidge tubes», completely replaced the troublesome cold cathode tubes by about 1920.
In about 1906, the physicist Charles Barkla discovered that X-rays could be scattered by gases, and that each element had a characteristic X-ray spectrum. He won the 1917 Nobel Prize in Physics for this discovery.
In 1912, Max von Laue, Paul Knipping, and Walter Friedrich first observed the diffraction of X-rays by crystals. This discovery, along with the early work of Paul Peter Ewald, William Henry Bragg, and William Lawrence Bragg, gave birth to the field of X-ray crystallography.[48]
In 1913, Henry Moseley performed crystallography experiments with X-rays emanating from various metals and formulated Moseley’s law which relates the frequency of the X-rays to the atomic number of the metal.
The Coolidge X-ray tube was invented the same year by William D. Coolidge. It made possible the continuous emissions of X-rays. Modern X-ray tubes are based on this design, often employing the use of rotating targets which allow for significantly higher heat dissipation than static targets, further allowing higher quantity X-ray output for use in high powered applications such as rotational CT scanners.
Chandra’s image of the galaxy cluster Abell 2125 reveals a complex of several massive multimillion-degree-Celsius gas clouds in the process of merging.
The use of X-rays for medical purposes (which developed into the field of radiation therapy) was pioneered by Major John Hall-Edwards in Birmingham, England. Then in 1908, he had to have his left arm amputated because of the spread of X-ray dermatitis on his arm.[49]
Medical science also used the motion picture to study human physiology. In 1913, a motion picture was made in Detroit showing a hard-boiled egg inside a human stomach. This early X-ray movie was recorded at a rate of one still image every four seconds.[50] Dr Lewis Gregory Cole of New York was a pioneer of the technique, which he called «serial radiography».[51][52] In 1918, X-rays were used in association with motion picture cameras to capture the human skeleton in motion.[53][54][55] In 1920, it was used to record the movements of tongue and teeth in the study of languages by the Institute of Phonetics in England.[56]
In 1914, Marie Curie developed radiological cars to support soldiers injured in World War I. The cars would allow for rapid X-ray imaging of wounded soldiers so battlefield surgeons could quickly and more accurately operate.[57]
From the early 1920s through to the 1950s, X-ray machines were developed to assist in the fitting of shoes[58] and were sold to commercial shoe stores.[59][60][61] Concerns regarding the impact of frequent or poorly controlled use were expressed in the 1950s,[62][63] leading to the practice’s eventual end that decade.[64]
The X-ray microscope was developed during the 1950s.
The Chandra X-ray Observatory, launched on July 23, 1999, has been allowing the exploration of the very violent processes in the universe which produce X-rays. Unlike visible light, which gives a relatively stable view of the universe, the X-ray universe is unstable. It features stars being torn apart by black holes, galactic collisions, and novae, and neutron stars that build up layers of plasma that then explode into space.
Phase-contrast X-ray image of a spider
An X-ray laser device was proposed as part of the Reagan Administration’s Strategic Defense Initiative in the 1980s, but the only test of the device (a sort of laser «blaster» or death ray, powered by a thermonuclear explosion) gave inconclusive results. For technical and political reasons, the overall project (including the X-ray laser) was defunded (though was later revived by the second Bush Administration as National Missile Defense using different technologies).
Phase-contrast X-ray imaging refers to a variety of techniques that use phase information of an X-ray beam to form the image. Due to its good sensitivity to density differences, it is especially useful for imaging soft tissues. It has become an important method for visualizing cellular and histological structures in a wide range of biological and medical studies. There are several technologies being used for X-ray phase-contrast imaging, all utilizing different principles to convert phase variations in the X-rays emerging from an object into intensity variations.[65][66] These include propagation-based phase contrast,[67] Talbot interferometry,[66] refraction-enhanced imaging,[68] and X-ray interferometry.[69] These methods provide higher contrast compared to normal absorption-based X-ray imaging, making it possible to distinguish from each other details that have almost similar density. A disadvantage is that these methods require more sophisticated equipment, such as synchrotron or microfocus X-ray sources, X-ray optics, and high resolution X-ray detectors.
Energy ranges[edit]
Soft and hard X-rays[edit]
X-rays with high photon energies above 5–10 keV (below 0.2–0.1 nm wavelength) are called hard X-rays, while those with lower energy (and longer wavelength) are called soft X-rays.[70] The intermediate range with photon energies of several keV is often referred to as tender X-rays. Due to their penetrating ability, hard X-rays are widely used to image the inside of objects, e.g., in medical radiography and airport security. The term X-ray is metonymically used to refer to a radiographic image produced using this method, in addition to the method itself. Since the wavelengths of hard X-rays are similar to the size of atoms, they are also useful for determining crystal structures by X-ray crystallography. By contrast, soft X-rays are easily absorbed in air; the attenuation length of 600 eV (~2 nm) X-rays in water is less than 1 micrometer.[71]
Gamma rays[edit]
There is no consensus for a definition distinguishing between X-rays and gamma rays. One common practice is to distinguish between the two types of radiation based on their source: X-rays are emitted by electrons, while gamma rays are emitted by the atomic nucleus.[72][73][74][75] This definition has several problems: other processes can also generate these high-energy photons, or sometimes the method of generation is not known. One common alternative is to distinguish X- and gamma radiation on the basis of wavelength (or, equivalently, frequency or photon energy), with radiation shorter than some arbitrary wavelength, such as 10−11 m (0.1 Å), defined as gamma radiation.[76] This criterion assigns a photon to an unambiguous category, but is only possible if wavelength is known. (Some measurement techniques do not distinguish between detected wavelengths.) However, these two definitions often coincide since the electromagnetic radiation emitted by X-ray tubes generally has a longer wavelength and lower photon energy than the radiation emitted by radioactive nuclei.[72] Occasionally, one term or the other is used in specific contexts due to historical precedent, based on measurement (detection) technique, or based on their intended use rather than their wavelength or source.
Thus, gamma-rays generated for medical and industrial uses, for example radiotherapy, in the ranges of 6–20 MeV, can in this context also be referred to as X-rays.[77]
Properties[edit]
Ionizing radiation hazard symbol
X-ray photons carry enough energy to ionize atoms and disrupt molecular bonds. This makes it a type of ionizing radiation, and therefore harmful to living tissue. A very high radiation dose over a short period of time causes radiation sickness, while lower doses can give an increased risk of radiation-induced cancer. In medical imaging, this increased cancer risk is generally greatly outweighed by the benefits of the examination. The ionizing capability of X-rays can be utilized in cancer treatment to kill malignant cells using radiation therapy. It is also used for material characterization using X-ray spectroscopy.
Hard X-rays can traverse relatively thick objects without being much absorbed or scattered. For this reason, X-rays are widely used to image the inside of visually opaque objects. The most often seen applications are in medical radiography and airport security scanners, but similar techniques are also important in industry (e.g., industrial radiography and industrial CT scanning) and research (e.g., small animal CT). The penetration depth varies with several orders of magnitude over the X-ray spectrum. This allows the photon energy to be adjusted for the application so as to give sufficient transmission through the object and at the same time provide good contrast in the image.
X-rays have much shorter wavelengths than visible light, which makes it possible to probe structures much smaller than can be seen using a normal microscope. This property is used in X-ray microscopy to acquire high-resolution images, and also in X-ray crystallography to determine the positions of atoms in crystals.
Interaction with matter[edit]
Attenuation length of X-rays in water showing the oxygen absorption edge at 540 eV, the energy−3 dependence of photoabsorption, as well as a leveling off at higher photon energies due to Compton scattering. The attenuation length is about four orders of magnitude longer for hard X-rays (right half) compared to soft X-rays (left half).
X-rays interact with matter in three main ways, through photoabsorption, Compton scattering, and Rayleigh scattering. The strength of these interactions depends on the energy of the X-rays and the elemental composition of the material, but not much on chemical properties, since the X-ray photon energy is much higher than chemical binding energies. Photoabsorption or photoelectric absorption is the dominant interaction mechanism in the soft X-ray regime and for the lower hard X-ray energies. At higher energies, Compton scattering dominates.
Photoelectric absorption[edit]
The probability of a photoelectric absorption per unit mass is approximately proportional to Z3/E3, where Z is the atomic number and E is the energy of the incident photon.[78] This rule is not valid close to inner shell electron binding energies where there are abrupt changes in interaction probability, so called absorption edges. However, the general trend of high absorption coefficients and thus short penetration depths for low photon energies and high atomic numbers is very strong. For soft tissue, photoabsorption dominates up to about 26 keV photon energy where Compton scattering takes over. For higher atomic number substances, this limit is higher. The high amount of calcium (Z = 20) in bones, together with their high density, is what makes them show up so clearly on medical radiographs.
A photoabsorbed photon transfers all its energy to the electron with which it interacts, thus ionizing the atom to which the electron was bound and producing a photoelectron that is likely to ionize more atoms in its path. An outer electron will fill the vacant electron position and produce either a characteristic X-ray or an Auger electron. These effects can be used for elemental detection through X-ray spectroscopy or Auger electron spectroscopy.
Compton scattering[edit]
Compton scattering is the predominant interaction between X-rays and soft tissue in medical imaging.[79] Compton scattering is an inelastic scattering of the X-ray photon by an outer shell electron. Part of the energy of the photon is transferred to the scattering electron, thereby ionizing the atom and increasing the wavelength of the X-ray. The scattered photon can go in any direction, but a direction similar to the original direction is more likely, especially for high-energy X-rays. The probability for different scattering angles is described by the Klein–Nishina formula. The transferred energy can be directly obtained from the scattering angle from the conservation of energy and momentum.
Rayleigh scattering[edit]
Rayleigh scattering is the dominant elastic scattering mechanism in the X-ray regime.[80] Inelastic forward scattering gives rise to the refractive index, which for X-rays is only slightly below 1.[81]
Production[edit]
Whenever charged particles (electrons or ions) of sufficient energy hit a material, X-rays are produced.
Production by electrons[edit]
| Anode material |
Atomic number |
Photon energy [keV] | Wavelength [nm] | ||
|---|---|---|---|---|---|
| Kα1 | Kβ1 | Kα1 | Kβ1 | ||
| W | 74 | 59.3 | 67.2 | 0.0209 | 0.0184 |
| Mo | 42 | 17.5 | 19.6 | 0.0709 | 0.0632 |
| Cu | 29 | 8.05 | 8.91 | 0.154 | 0.139 |
| Ag | 47 | 22.2 | 24.9 | 0.0559 | 0.0497 |
| Ga | 31 | 9.25 | 10.26 | 0.134 | 0.121 |
| In | 49 | 24.2 | 27.3 | 0.0512 | 0.0455 |
X-rays can be generated by an X-ray tube, a vacuum tube that uses a high voltage to accelerate the electrons released by a hot cathode to a high velocity. The high velocity electrons collide with a metal target, the anode, creating the X-rays.[84] In medical X-ray tubes the target is usually tungsten or a more crack-resistant alloy of rhenium (5%) and tungsten (95%), but sometimes molybdenum for more specialized applications, such as when softer X-rays are needed as in mammography. In crystallography, a copper target is most common, with cobalt often being used when fluorescence from iron content in the sample might otherwise present a problem.
The maximum energy of the produced X-ray photon is limited by the energy of the incident electron, which is equal to the voltage on the tube times the electron charge, so an 80 kV tube cannot create X-rays with an energy greater than 80 keV. When the electrons hit the target, X-rays are created by two different atomic processes:
- Characteristic X-ray emission (X-ray electroluminescence): If the electron has enough energy, it can knock an orbital electron out of the inner electron shell of the target atom. After that, electrons from higher energy levels fill the vacancies, and X-ray photons are emitted. This process produces an emission spectrum of X-rays at a few discrete frequencies, sometimes referred to as spectral lines. Usually, these are transitions from the upper shells to the K shell (called K lines), to the L shell (called L lines) and so on. If the transition is from 2p to 1s, it is called Kα, while if it is from 3p to 1s it is Kβ. The frequencies of these lines depend on the material of the target and are therefore called characteristic lines. The Kα line usually has greater intensity than the Kβ one and is more desirable in diffraction experiments. Thus the Kβ line is filtered out by a filter. The filter is usually made of a metal having one proton less than the anode material (e.g., Ni filter for Cu anode or Nb filter for Mo anode).
- Bremsstrahlung: This is radiation given off by the electrons as they are scattered by the strong electric field near the high-Z (proton number) nuclei. These X-rays have a continuous spectrum. The frequency of Bremsstrahlung is limited by the energy of incident electrons.
So, the resulting output of a tube consists of a continuous Bremsstrahlung spectrum falling off to zero at the tube voltage, plus several spikes at the characteristic lines. The voltages used in diagnostic X-ray tubes range from roughly 20 kV to 150 kV and thus the highest energies of the X-ray photons range from roughly 20 keV to 150 keV.[85]
Both of these X-ray production processes are inefficient, with only about one percent of the electrical energy used by the tube converted into X-rays, and thus most of the electric power consumed by the tube is released as waste heat. When producing a usable flux of X-rays, the X-ray tube must be designed to dissipate the excess heat.
A specialized source of X-rays which is becoming widely used in research is synchrotron radiation, which is generated by particle accelerators. Its unique features are X-ray outputs many orders of magnitude greater than those of X-ray tubes, wide X-ray spectra, excellent collimation, and linear polarization.[86]
Short nanosecond bursts of X-rays peaking at 15 keV in energy may be reliably produced by peeling pressure-sensitive adhesive tape from its backing in a moderate vacuum. This is likely to be the result of recombination of electrical charges produced by triboelectric charging. The intensity of X-ray triboluminescence is sufficient for it to be used as a source for X-ray imaging.[87]
Production by fast positive ions[edit]
X-rays can also be produced by fast protons or other positive ions. The proton-induced X-ray emission or particle-induced X-ray emission is widely used as an analytical procedure. For high energies, the production cross section is proportional to Z12Z2−4, where Z1 refers to the atomic number of the ion, Z2 refers to that of the target atom.[88] An overview of these cross sections is given in the same reference.
Production in lightning and laboratory discharges[edit]
X-rays are also produced in lightning accompanying terrestrial gamma-ray flashes. The underlying mechanism is the acceleration of electrons in lightning related electric fields and the subsequent production of photons through Bremsstrahlung.[89] This produces photons with energies of some few keV and several tens of MeV.[90] In laboratory discharges with a gap size of approximately 1 meter length and a peak voltage of 1 MV, X-rays with a characteristic energy of 160 keV are observed.[91] A possible explanation is the encounter of two streamers and the production of high-energy run-away electrons;[92] however, microscopic simulations have shown that the duration of electric field enhancement between two streamers is too short to produce a significant number of run-away electrons.[93] Recently, it has been proposed that air perturbations in the vicinity of streamers can facilitate the production of run-away electrons and hence of X-rays from discharges.[94][95]
Detectors[edit]
X-ray detectors vary in shape and function depending on their purpose. Imaging detectors such as those used for radiography were originally based on photographic plates and later photographic film, but are now mostly replaced by various digital detector types such as image plates and flat panel detectors. For radiation protection direct exposure hazard is often evaluated using ionization chambers, while dosimeters are used to measure the radiation dose a person has been exposed to. X-ray spectra can be measured either by energy dispersive or wavelength dispersive spectrometers. For X-ray diffraction applications, such as X-ray crystallography, hybrid photon counting detectors are widely used.[96]
Medical uses[edit]
Patient undergoing an x-ray exam in a hospital radiology room.
Since Röntgen’s discovery that X-rays can identify bone structures, X-rays have been used for medical imaging.[97] The first medical use was less than a month after his paper on the subject.[34] Up to 2010, five billion medical imaging examinations had been conducted worldwide.[98] Radiation exposure from medical imaging in 2006 made up about 50% of total ionizing radiation exposure in the United States.[99]
Projectional radiographs[edit]
Plain radiograph of the right knee
Projectional radiography is the practice of producing two-dimensional images using X-ray radiation. Bones contain a high concentration of calcium, which, due to its relatively high atomic number, absorbs X-rays efficiently. This reduces the amount of X-rays reaching the detector in the shadow of the bones, making them clearly visible on the radiograph. The lungs and trapped gas also show up clearly because of lower absorption compared to tissue, while differences between tissue types are harder to see.
Projectional radiographs are useful in the detection of pathology of the skeletal system as well as for detecting some disease processes in soft tissue. Some notable examples are the very common chest X-ray, which can be used to identify lung diseases such as pneumonia, lung cancer, or pulmonary edema, and the abdominal x-ray, which can detect bowel (or intestinal) obstruction, free air (from visceral perforations), and free fluid (in ascites). X-rays may also be used to detect pathology such as gallstones (which are rarely radiopaque) or kidney stones which are often (but not always) visible. Traditional plain X-rays are less useful in the imaging of soft tissues such as the brain or muscle. One area where projectional radiographs are used extensively is in evaluating how an orthopedic implant, such as a knee, hip or shoulder replacement, is situated in the body with respect to the surrounding bone. This can be assessed in two dimensions from plain radiographs, or it can be assessed in three dimensions if a technique called ‘2D to 3D registration’ is used. This technique purportedly negates projection errors associated with evaluating implant position from plain radiographs.[100]
Dental radiography is commonly used in the diagnoses of common oral problems, such as cavities.
In medical diagnostic applications, the low energy (soft) X-rays are unwanted, since they are totally absorbed by the body, increasing the radiation dose without contributing to the image. Hence, a thin metal sheet, often of aluminium, called an X-ray filter, is usually placed over the window of the X-ray tube, absorbing the low energy part in the spectrum. This is called hardening the beam since it shifts the center of the spectrum towards higher energy (or harder) X-rays.
To generate an image of the cardiovascular system, including the arteries and veins (angiography) an initial image is taken of the anatomical region of interest. A second image is then taken of the same region after an iodinated contrast agent has been injected into the blood vessels within this area. These two images are then digitally subtracted, leaving an image of only the iodinated contrast outlining the blood vessels. The radiologist or surgeon then compares the image obtained to normal anatomical images to determine whether there is any damage or blockage of the vessel.
Computed tomography[edit]
Computed tomography (CT scanning) is a medical imaging modality where tomographic images or slices of specific areas of the body are obtained from a large series of two-dimensional X-ray images taken in different directions.[101] These cross-sectional images can be combined into a three-dimensional image of the inside of the body and used for diagnostic and therapeutic purposes in various medical disciplines.
Fluoroscopy[edit]
Fluoroscopy is an imaging technique commonly used by physicians or radiation therapists to obtain real-time moving images of the internal structures of a patient through the use of a fluoroscope. In its simplest form, a fluoroscope consists of an X-ray source and a fluorescent screen, between which a patient is placed. However, modern fluoroscopes couple the screen to an X-ray image intensifier and CCD video camera allowing the images to be recorded and played on a monitor. This method may use a contrast material. Examples include cardiac catheterization (to examine for coronary artery blockages) and barium swallow (to examine for esophageal disorders and swallowing disorders).
Radiotherapy[edit]
The use of X-rays as a treatment is known as radiation therapy and is largely used for the management (including palliation) of cancer; it requires higher radiation doses than those received for imaging alone. X-rays beams are used for treating skin cancers using lower energy X-ray beams while higher energy beams are used for treating cancers within the body such as brain, lung, prostate, and breast.[102][103]
Adverse effects[edit]
Abdominal radiograph of a pregnant woman, a procedure that should be performed only after proper assessment of benefit versus risk
Diagnostic X-rays (primarily from CT scans due to the large dose used) increase the risk of developmental problems and cancer in those exposed.[104][105][106] X-rays are classified as a carcinogen by both the World Health Organization’s International Agency for Research on Cancer and the U.S. government.[98][107] It is estimated that 0.4% of current cancers in the United States are due to computed tomography (CT scans) performed in the past and that this may increase to as high as 1.5–2% with 2007 rates of CT usage.[108]
Experimental and epidemiological data currently do not support the proposition that there is a threshold dose of radiation below which there is no increased risk of cancer.[109] However, this is under increasing doubt.[110] Cancer risk can start at the exposure of 1100 mGy.[111] It is estimated that the additional radiation from diagnostic X-rays will increase the average person’s cumulative risk of getting cancer by age 75 by 0.6–3.0%.[112] The amount of absorbed radiation depends upon the type of X-ray test and the body part involved.[108] CT and fluoroscopy entail higher doses of radiation than do plain X-rays.
To place the increased risk in perspective, a plain chest X-ray will expose a person to the same amount from background radiation that people are exposed to (depending upon location) every day over 10 days, while exposure from a dental X-ray is approximately equivalent to 1 day of environmental background radiation.[113] Each such X-ray would add less than 1 per 1,000,000 to the lifetime cancer risk. An abdominal or chest CT would be the equivalent to 2–3 years of background radiation to the whole body, or 4–5 years to the abdomen or chest, increasing the lifetime cancer risk between 1 per 1,000 to 1 per 10,000.[113] This is compared to the roughly 40% chance of a US citizen developing cancer during their lifetime.[114] For instance, the effective dose to the torso from a CT scan of the chest is about 5 mSv, and the absorbed dose is about 14 mGy.[115] A head CT scan (1.5 mSv, 64 mGy)[116] that is performed once with and once without contrast agent, would be equivalent to 40 years of background radiation to the head. Accurate estimation of effective doses due to CT is difficult with the estimation uncertainty range of about ±19% to ±32% for adult head scans depending upon the method used.[117]
The risk of radiation is greater to a fetus, so in pregnant patients, the benefits of the investigation (X-ray) should be balanced with the potential hazards to the fetus.[118][119] If there is 1 scan in 9 months, it can be harmful to the fetus.[120] Therefore, women who are pregnant get ultrasounds as their diagnostic imaging because this does not use radiation.[120] If there is too much radiation exposure there could be harmful effects on the fetus or the reproductive organs of the mother.[120] In the US, there are an estimated 62 million CT scans performed annually, including more than 4 million on children.[108] Avoiding unnecessary X-rays (especially CT scans) reduces radiation dose and any associated cancer risk.[121]
Medical X-rays are a significant source of human-made radiation exposure. In 1987, they accounted for 58% of exposure from human-made sources in the United States. Since human-made sources accounted for only 18% of the total radiation exposure, most of which came from natural sources (82%), medical X-rays only accounted for 10% of total American radiation exposure; medical procedures as a whole (including nuclear medicine) accounted for 14% of total radiation exposure. By 2006, however, medical procedures in the United States were contributing much more ionizing radiation than was the case in the early 1980s. In 2006, medical exposure constituted nearly half of the total radiation exposure of the U.S. population from all sources. The increase is traceable to the growth in the use of medical imaging procedures, in particular computed tomography (CT), and to the growth in the use of nuclear medicine.[99][122]
Dosage due to dental X-rays varies significantly depending on the procedure and the technology (film or digital). Depending on the procedure and the technology, a single dental X-ray of a human results in an exposure of 0.5 to 4 mrem. A full mouth series of X-rays may result in an exposure of up to 6 (digital) to 18 (film) mrem, for a yearly average of up to 40 mrem.[123][124][125][126][127][128][129]
Financial incentives have been shown to have a significant impact on X-ray use with doctors who are paid a separate fee for each X-ray providing more X-rays.[130]
Early photon tomography or EPT[131] (as of 2015) along with other techniques[132] are being researched as potential alternatives to X-rays for imaging applications.
Other uses[edit]
Other notable uses of X-rays include:
Each dot, called a reflection, in this diffraction pattern forms from the constructive interference of scattered X-rays passing through a crystal. The data can be used to determine the crystalline structure.
- X-ray crystallography in which the pattern produced by the diffraction of X-rays through the closely spaced lattice of atoms in a crystal is recorded and then analysed to reveal the nature of that lattice. A related technique, fiber diffraction, was used by Rosalind Franklin to discover the double helical structure of DNA.[133]
- X-ray astronomy, which is an observational branch of astronomy, which deals with the study of X-ray emission from celestial objects.
- X-ray microscopic analysis, which uses electromagnetic radiation in the soft X-ray band to produce images of very small objects.
- X-ray fluorescence, a technique in which X-rays are generated within a specimen and detected. The outgoing energy of the X-ray can be used to identify the composition of the sample.
- Industrial radiography uses X-rays for inspection of industrial parts, particularly welds.
- Radiography of cultural objects, most often x-rays of paintings to reveal underdrawing, pentimenti alterations in the course of painting or by later restorers, and sometimes previous paintings on the support. Many pigments such as lead white show well in radiographs.
- X-ray spectromicroscopy has been used to analyse the reactions of pigments in paintings. For example, in analysing colour degradation in the paintings of van Gogh.[134]
Using X-ray for inspection and quality control: the differences in the structures of the die and bond wires reveal the left chip to be counterfeit.[135]
- Authentication and quality control of packaged items.
- Industrial CT (computed tomography), a process that uses X-ray equipment to produce three-dimensional representations of components both externally and internally. This is accomplished through computer processing of projection images of the scanned object in many directions.
- Airport security luggage scanners use X-rays for inspecting the interior of luggage for security threats before loading on aircraft.
- Border control truck scanners and domestic police departments use X-rays for inspecting the interior of trucks.
- X-ray art and fine art photography, artistic use of X-rays, for example the works by Stane Jagodič
- X-ray hair removal, a method popular in the 1920s but now banned by the FDA.[136]
- Shoe-fitting fluoroscopes were popularized in the 1920s, banned in the US in the 1960s, in the UK in the 1970s, and later in continental Europe.
- Roentgen stereophotogrammetry is used to track movement of bones based on the implantation of markers
- X-ray photoelectron spectroscopy is a chemical analysis technique relying on the photoelectric effect, usually employed in surface science.
- Radiation implosion is the use of high energy X-rays generated from a fission explosion (an A-bomb) to compress nuclear fuel to the point of fusion ignition (an H-bomb).
Visibility[edit]
While generally considered invisible to the human eye, in special circumstances X-rays can be visible. Brandes, in an experiment a short time after Röntgen’s landmark 1895 paper, reported after dark adaptation and placing his eye close to an X-ray tube, seeing a faint «blue-gray» glow which seemed to originate within the eye itself.[137] Upon hearing this, Röntgen reviewed his record books and found he too had seen the effect. When placing an X-ray tube on the opposite side of a wooden door Röntgen had noted the same blue glow, seeming to emanate from the eye itself, but thought his observations to be spurious because he only saw the effect when he used one type of tube. Later he realized that the tube which had created the effect was the only one powerful enough to make the glow plainly visible and the experiment was thereafter readily repeatable. The knowledge that X-rays are actually faintly visible to the dark-adapted naked eye has largely been forgotten today; this is probably due to the desire not to repeat what would now be seen as a recklessly dangerous and potentially harmful experiment with ionizing radiation. It is not known what exact mechanism in the eye produces the visibility: it could be due to conventional detection (excitation of rhodopsin molecules in the retina), direct excitation of retinal nerve cells, or secondary detection via, for instance, X-ray induction of phosphorescence in the eyeball with conventional retinal detection of the secondarily produced visible light.
Though X-rays are otherwise invisible, it is possible to see the ionization of the air molecules if the intensity of the X-ray beam is high enough. The beamline from the wiggler at the European Synchrotron Radiation Facility[138] is one example of such high intensity.[139]
Units of measure and exposure[edit]
The measure of X-rays ionizing ability is called the exposure:
- The coulomb per kilogram (C/kg) is the SI unit of ionizing radiation exposure, and it is the amount of radiation required to create one coulomb of charge of each polarity in one kilogram of matter.
- The roentgen (R) is an obsolete traditional unit of exposure, which represented the amount of radiation required to create one electrostatic unit of charge of each polarity in one cubic centimeter of dry air. 1 roentgen = 2.58×10−4 C/kg.
However, the effect of ionizing radiation on matter (especially living tissue) is more closely related to the amount of energy deposited into them rather than the charge generated. This measure of energy absorbed is called the absorbed dose:
- The gray (Gy), which has units of (joules/kilogram), is the SI unit of absorbed dose, and it is the amount of radiation required to deposit one joule of energy in one kilogram of any kind of matter.
- The rad is the (obsolete) corresponding traditional unit, equal to 10 millijoules of energy deposited per kilogram. 100 rad = 1 gray.
The equivalent dose is the measure of the biological effect of radiation on human tissue. For X-rays it is equal to the absorbed dose.
- The Roentgen equivalent man (rem) is the traditional unit of equivalent dose. For X-rays it is equal to the rad, or, in other words, 10 millijoules of energy deposited per kilogram. 100 rem = 1 Sv.
- The sievert (Sv) is the SI unit of equivalent dose, and also of effective dose. For X-rays the «equivalent dose» is numerically equal to a Gray (Gy). 1 Sv = 1 Gy. For the «effective dose» of X-rays, it is usually not equal to the Gray (Gy).
| Quantity | Unit | Symbol | Derivation | Year | SI equivalent |
|---|---|---|---|---|---|
| Activity (A) | becquerel | Bq | s−1 | 1974 | SI unit |
| curie | Ci | 3.7 × 1010 s−1 | 1953 | 3.7×1010 Bq | |
| rutherford | Rd | 106 s−1 | 1946 | 1,000,000 Bq | |
| Exposure (X) | coulomb per kilogram | C/kg | C⋅kg−1 of air | 1974 | SI unit |
| röntgen | R | esu / 0.001293 g of air | 1928 | 2.58 × 10−4 C/kg | |
| Absorbed dose (D) | gray | Gy | J⋅kg−1 | 1974 | SI unit |
| erg per gram | erg/g | erg⋅g−1 | 1950 | 1.0 × 10−4 Gy | |
| rad | rad | 100 erg⋅g−1 | 1953 | 0.010 Gy | |
| Equivalent dose (H) | sievert | Sv | J⋅kg−1 × WR | 1977 | SI unit |
| röntgen equivalent man | rem | 100 erg⋅g−1 x WR | 1971 | 0.010 Sv | |
| Effective dose (E) | sievert | Sv | J⋅kg−1 × WR × WT | 1977 | SI unit |
| röntgen equivalent man | rem | 100 erg⋅g−1 × WR × WT | 1971 | 0.010 Sv |
See also[edit]
References[edit]
- ^ «X-Rays». Science Mission Directorate. NASA.
- ^ Novelline, Robert (1997). Squire’s Fundamentals of Radiology. Harvard University Press. 5th edition. ISBN 0-674-83339-2.
- ^ «X-ray». Oxford English Dictionary (Online ed.). Oxford University Press. (Subscription or participating institution membership required.)
- ^ Filler A (2009). «The History, Development and Impact of Computed Imaging in Neurological Diagnosis and Neurosurgery: CT, MRI, and DTI». Nature Precedings. doi:10.1038/npre.2009.3267.5.
- ^ Morgan W (1785-02-24). «Electrical Experiments Made in Order to Ascertain the Non-Conducting Power of a Perfect Vacuum, &c». Philosophical Transactions of the Royal Society. Royal Society of London. 75: 272–278. doi:10.1098/rstl.1785.0014.
- ^ Anderson JG (January 1945). «William Morgan and X-rays». Transactions of the Faculty of Actuaries. 17: 219–221. doi:10.1017/s0071368600003001.
- ^ Wyman T (Spring 2005). «Fernando Sanford and the Discovery of X-rays». «Imprint», from the Associates of the Stanford University Libraries: 5–15.
- ^ Thomson JJ (1903). The Discharge of Electricity through Gasses. USA: Charles Scribner’s Sons. pp. 182–186.
- ^ Mayba II, Gaida R, Kyle RA, Shampo MA (July 1997). «Ukrainian physicist contributes to the discovery of X-rays». Mayo Clinic Proceedings. Mayo Foundation for Medical Education and Research. 72 (7): 658. doi:10.1016/s0025-6196(11)63573-8. PMID 9212769. Archived from the original on 2008-05-28. Retrieved 2008-04-06.
- ^ Wiedmann’s Annalen, Vol. XLVIII.
- ^ a b Hrabak M, Padovan RS, Kralik M, Ozretic D, Potocki K (July 2008). «Scenes from the past: Nikola Tesla and the discovery of X-rays». Radiographics. 28 (4): 1189–1192. doi:10.1148/rg.284075206. PMID 18635636.
- ^ Chadda PK (2009). Hydroenergy and Its Energy Potential. Pinnacle Technology. p. 88. ISBN 978-1-61820-149-2.
- ^ Tesla’s technical publications indicate that he invented and developed a single-electrode X-ray tube. Morton, William James and Hammer, Edwin W. (1896) American Technical Book Co., p. 68. U.S. Patent 514,170, «Incandescent Electric Light». U.S. Patent 454,622 «System of Electric Lighting». These differed from other X-ray tubes in having no target electrode and worked with the output of a Tesla coil.
- ^ Stanton A (1896-01-23). «Wilhelm Conrad Röntgen On a New Kind of Rays: translation of a paper read before the Würzburg Physical and Medical Society, 1895». Nature. 53 (1369): 274–6. Bibcode:1896Natur..53R.274.. doi:10.1038/053274b0. see also pp. 268 and 276 of the same issue.
- ^ Garcia, J.; Buchwald, N. A.; Feder, B. H.; Koelling, R. A.; Tedrow, L. (1964). «Sensitivity of the head to X-ray». Science. 144 (3625): 1470–1472. doi:10.1126/science.144.3625.1470. ISSN 0036-8075. PMID 14171545. S2CID 44719943.
Rats have been trained to respond to signals consisting of very low doses of chi-ray directed to the head.
- ^ Baganha, M. F.; Marques, M. A.; Botelho, M. F.; Teixeira, M. L.; Carvalheira, V.; Calisto, J.; Silva, A.; Fernandes, A.; Torres, M.; Brito, J. (1993). «Tomodensitometry and radioisotopic methods in the study of unilateral lung hyperlucencies of vascular origin». Acta Médica Portuguesa. 6 (1): 19–24. ISSN 0870-399X. PMID 8475784.
- ^ Takahashi, K.; Case, B. W.; Dufresne, A.; Fraser, R.; Higashi, T.; Siemiatycki, J. (1994). «Relation between lung asbestos fibre burden and exposure indices based on job history». Occupational and Environmental Medicine. 51 (7): 461–469. doi:10.1136/oem.51.7.461. ISSN 1351-0711. PMC 1128015. PMID 8044245.
- ^ Karlsson EB (9 February 2000). «The Nobel Prizes in Physics 1901–2000». Stockholm: The Nobel Foundation. Retrieved 24 November 2011.
- ^ Peters P (1995). «W. C. Roentgen and the discovery of x-rays». Textbook of Radiology. Medcyclopedia.com, GE Healthcare. Archived from the original on 11 May 2008. Retrieved 5 May 2008.
- ^ Glasser O (1993). Wilhelm Conrad Röntgen and the early history of the roentgen rays. Norman Publishing. pp. 10–15. ISBN 978-0930405229.
- ^ Arthur C (2010-11-08). «Google doodle celebrates 115 years of X-rays». The Guardian. Guardian US. Retrieved 5 February 2019.
- ^ Kevles BH (1996). Naked to the Bone Medical Imaging in the Twentieth Century. Camden, NJ: Rutgers University Press. pp. 19–22. ISBN 978-0-8135-2358-3.
- ^ Sample S (2007-03-27). «X-Rays». The Electromagnetic Spectrum. NASA. Retrieved 2007-12-03.
- ^ Markel H (20 December 2012). «‘I Have Seen My Death’: How the World Discovered the X-Ray». PBS NewsHour. PBS. Retrieved 23 March 2019.
- ^ Glasser O (1958). Dr. W. C. Ro ̈ntgen. Springfield: Thomas.
- ^ Natale S (2011-11-01). «The Invisible Made Visible». Media History. 17 (4): 345–358. doi:10.1080/13688804.2011.602856. hdl:2134/19408. S2CID 142518799.
- ^ Natale S (2011-08-04). «A Cosmology of Invisible Fluids: Wireless, X-Rays, and Psychical Research Around 1900». Canadian Journal of Communication. 36 (2): 263–276. doi:10.22230/cjc.2011v36n2a2368.
- ^ Grove AW (1997-01-01). «Röntgen’s ghosts: photography, X-rays, and the Victorian imagination». Literature and Medicine. 16 (2): 141–173. doi:10.1353/lm.1997.0016. PMID 9368224. S2CID 35604474.
- ^ a b c d e f Feldman A (November 1989). «A sketch of the technical history of radiology from 1896 to 1920». Radiographics. 9 (6): 1113–1128. doi:10.1148/radiographics.9.6.2685937. PMID 2685937.
- ^ «Major John Hall-Edwards». Birmingham City Council. Archived from the original on September 28, 2012. Retrieved 2012-05-17.
- ^ Kudriashov, Y. B. (2008). Radiation Biophysics. Nova Publishers. p. xxi. ISBN 9781600212802.
- ^ «Green, James (Zoological Artist), Sciagraphs of British batrachians and reptiles, 1897». Yale Centre for British Art. Retrieved 24 November 2021.
- ^ «Sciagraphs of British Batrachians and Reptiles1». Nature. 55 (1432): 539–540. 1 April 1897. Bibcode:1897Natur..55..539.. doi:10.1038/055539a0. S2CID 4054184.
- ^ a b Spiegel PK (January 1995). «The first clinical X-ray made in America—100 years». AJR. American Journal of Roentgenology. 164 (1): 241–243. doi:10.2214/ajr.164.1.7998549. PMID 7998549.
- ^ Nicolaas A. Rupke, Eminent Lives in Twentieth-Century Science and Religion, page 300, Peter Lang, 2009 ISBN 3631581203
- ^ «Visible Proofs: Forensic Views of the Body: Galleries: Cases: Could X-rays Have Saved President William McKinley?». www.nlm.nih.gov. Retrieved 2022-01-24.
- ^ Daniel J (April 1896). «THE X-RAYS». Science. 3 (67): 562–563. Bibcode:1896Sci…..3..562D. doi:10.1126/science.3.67.562. PMID 17779817.
- ^ Fleming WL (1909). The South in the Building of the Nation: Biography A-J. Pelican Publishing. p. 300. ISBN 978-1589809468.
- ^ Ce4Rt (Mar 2014). Understanding Ionizing Radiation and Protection. p. 174.
- ^ Glasser O (1934). Wilhelm Conrad Röntgen and the Early History of the Roentgen Rays. Norman Publishing. p. 294. ISBN 978-0930405229.
- ^ Sansare K, Khanna V, Karjodkar F (February 2011). «Early victims of X-rays: a tribute and current perception». Dento Maxillo Facial Radiology. 40 (2): 123–125. doi:10.1259/dmfr/73488299. PMC 3520298. PMID 21239576.
- ^ a b «ISU Health Physics Radinf — First 50 Years». sites.google.com. Retrieved 2022-01-24.
- ^ California, San Francisco Area Funeral Home Records, 1835–1979. Database with images. FamilySearch. Jacob Fleischman in the entry for Elizabeth Aschheim. 03 Aug 1905. Citing funeral home J.S. Godeau, San Francisco, San Francisco, California. Record book Vol. 06, p. 1–400, 1904–1906. San Francisco Public Library. San Francisco History and Archive Center.
- ^ Editor. (August 5, 1905). Aschheim. Obituaries. San Francisco Examiner. San Francisco, California.
- ^ Editor. (August 5, 1905). Obituary Notice. Elizabeth Fleischmann. San Francisco Chronicle. Page 10.
- ^ «Major John Hall-Edwards». Birmingham City Council. Archived from the original on 28 September 2012. Retrieved 23 April 2010.
- ^ a b Schall K (1905). Electro-medical Instruments and their Management. Bemrose & Sons Ltd. Printers. pp. 96, 107.
- ^ Stoddart C (1 March 2022). «Structural biology: How proteins got their close-up». Knowable Magazine. doi:10.1146/knowable-022822-1. Retrieved 25 March 2022.
- ^ Birmingham City Council: Major John Hall-Edwards Archived September 28, 2012, at the Wayback Machine
- ^ «X-ray movies show hard boiled egg fighting digestive organs (1913)». The News-Palladium. 1913-04-04. p. 2. Retrieved 2020-11-26.
- ^ «X-ray moving pictures latest (1913)». Chicago Tribune. 1913-06-22. p. 32. Retrieved 2020-11-26.
- ^ «Homeopaths to show movies of body’s organs at work (1915)». The Central New Jersey Home News. 1915-05-10. p. 6. Retrieved 2020-11-26.
- ^ «How X-Ray Movies Are Taken (1918)». Davis County Clipper. 1918-03-15. p. 2. Retrieved 2020-11-26.
- ^ «X-ray movies (1919)». Tampa Bay Times. 1919-01-12. p. 16. Retrieved 2020-11-26.
- ^ «X-ray movies perfected. Will show motions of bones and joints of human body. (1918)». The Sun. 1918-01-07. p. 7. Retrieved 2020-11-26.
- ^ «Talk is cheap? X-ray used by Institute of Phonetics (1920)». New Castle Herald. 1920-01-02. p. 13. Retrieved 2020-11-26.
- ^ Jorgensen TJ (10 October 2017). «Marie Curie and her X-ray vehicles’ contribution to World War I battlefield medicine». The Conversation. Retrieved February 23, 2018.
- ^ «X-Rays for Fitting Boots». Warwick Daily News (Qld.: 1919–1954). 1921-08-25. p. 4. Retrieved 2020-11-27.
- ^ «T. C. BEIRNE’S X-RAY SHOE FITTING». Telegraph (Brisbane, Qld. : 1872–1947). 1925-07-17. p. 8. Retrieved 2017-11-05.
- ^ «THE PEDOSCOPE». Sunday Times (Perth, WA : 1902–1954). 1928-07-15. p. 5. Retrieved 2017-11-05.
- ^ «X-RAY SHOE FITTINGS». Biz (Fairfield, NSW : 1928–1972). 1955-07-27. p. 10. Retrieved 2017-11-05.
- ^ «SHOE X-RAY DANGERS». Brisbane Telegraph (Qld. : 1948–1954). 1951-02-28. p. 7. Retrieved 2017-11-05.
- ^ «X-ray shoe sets in S.A. ‘controlled’«. News (Adelaide, SA : 1923–1954). 1951-04-27. p. 12. Retrieved 2017-11-05.
- ^ «Ban On Shoe X-ray Machines Resented». Canberra Times (ACT : 1926–1995). 1957-06-26. p. 4. Retrieved 2017-11-05.
- ^ Fitzgerald R (2000). «Phase-sensitive x-ray imaging». Physics Today. 53 (7): 23–26. Bibcode:2000PhT….53g..23F. doi:10.1063/1.1292471. S2CID 121322301.
- ^ a b David C, Nöhammer B, Solak H, Ziegler (2002). «Differential x-ray phase contrast imaging using a shearing interferometer». Applied Physics Letters. 81 (17): 3287–3289. Bibcode:2002ApPhL..81.3287D. doi:10.1063/1.1516611.
- ^ Wilkins SW, Gureyev TE, Gao D, Pogany A, Stevenson AW (1996). «Phase-contrast imaging using polychromatic hard X-rays». Nature. 384 (6607): 335–338. Bibcode:1996Natur.384..335W. doi:10.1038/384335a0. S2CID 4273199.
- ^ Davis TJ, Gao D, Gureyev TE, Stevenson AW, Wilkins SW (1995). «Phase-contrast imaging of weakly absorbing materials using hard X-rays». Nature. 373 (6515): 595–598. Bibcode:1995Natur.373..595D. doi:10.1038/373595a0. S2CID 4287341.
- ^ Momose A, Takeda T, Itai Y, Hirano K (April 1996). «Phase-contrast X-ray computed tomography for observing biological soft tissues». Nature Medicine. 2 (4): 473–475. doi:10.1038/nm0496-473. PMID 8597962. S2CID 23523144.
- ^ Attwood, David (1999). Soft X-rays and extreme ultraviolet radiation. Cambridge University. p. 2. ISBN 978-0-521-65214-8. Archived from the original on 2012-11-11. Retrieved 2012-11-04.
- ^ «Physics.nist.gov». Physics.nist.gov. Retrieved 2011-11-08.
- ^ a b Denny PP, Heaton B (1999). Physics for Diagnostic Radiology. USA: CRC Press. p. 12. ISBN 978-0-7503-0591-4.
- ^ Feynman R, Leighton R, Sands M (1963). The Feynman Lectures on Physics. Vol. 1. USA: Addison-Wesley. pp. 2–5. ISBN 978-0-201-02116-5.
- ^ L’Annunziata M, Abrade M (2003). Handbook of Radioactivity Analysis. Academic Press. p. 58. ISBN 978-0-12-436603-9.
- ^ Grupen C, Cowan G, Eidelman SD, Stroh T (2005). Astroparticle Physics. Springer. p. 109. ISBN 978-3-540-25312-9.
- ^ Hodgman, Charles, ed. (1961). CRC Handbook of Chemistry and Physics, 44th Ed. USA: Chemical Rubber Co. p. 2850.
- ^ Government of Canada, Canadian Centre for Occupational Health and Safety (2019-05-09). «Radiation – Quantities and Units of Ionizing Radiation: OSH Answers». www.ccohs.ca. Retrieved 2019-05-09.
- ^ Bushberg, Jerrold T.; Seibert, J. Anthony; Leidholdt, Edwin M.; Boone, John M. (2002). The essential physics of medical imaging. Lippincott Williams & Wilkins. p. 42. ISBN 978-0-683-30118-2.
- ^ Bushberg, Jerrold T.; Seibert, J. Anthony; Leidholdt, Edwin M.; Boone, John M. (2002). The essential physics of medical imaging. Lippincott Williams & Wilkins. p. 38. ISBN 978-0-683-30118-2.
- ^ Kissel L (2000-09-02). «RTAB: the Rayleigh scattering database». Radiation Physics and Chemistry. Lynn Kissel. 59 (2): 185–200. Bibcode:2000RaPC…59..185K. doi:10.1016/S0969-806X(00)00290-5. Archived from the original on 2011-12-12. Retrieved 2012-11-08.
- ^ Attwood, David (1999). «3». Soft X-rays and extreme ultraviolet radiation. Cambridge University Press. ISBN 978-0-521-65214-8. Archived from the original on 2012-11-11. Retrieved 2012-11-04.
- ^ «X-ray Transition Energies Database». NIST Physical Measurement Laboratory. 2011-12-09. Retrieved 2016-02-19.
- ^ «X-Ray Data Booklet Table 1-3» (PDF). Center for X-ray Optics and Advanced Light Source, Lawrence Berkeley National Laboratory. 2009-10-01. Archived from the original (PDF) on 23 April 2009. Retrieved 2016-02-19.
- ^ Whaites E, Cawson R (2002). Essentials of Dental Radiography and Radiology. Elsevier Health Sciences. pp. 15–20. ISBN 978-0-443-07027-3.
- ^ Bushburg J, Seibert A, Leidholdt E, Boone J (2002). The Essential Physics of Medical Imaging. USA: Lippincott Williams & Wilkins. p. 116. ISBN 978-0-683-30118-2.
- ^ Emilio B, Ballerna A (1994). «Preface». Biomedical Applications of Synchrotron Radiation: Proceedings of the 128th Course at the International School of Physics -Enrico Fermi- 12–22 July 1994, Varenna, Italy. IOS Press. p. xv. ISBN 90-5199-248-3.
- ^ Camara CG, Escobar JV, Hird JR, Putterman SJ (2008). «Correlation between nanosecond X-ray flashes and stick–slip friction in peeling tape» (PDF). Nature. 455 (7216): 1089–1092. Bibcode:2008Natur.455.1089C. doi:10.1038/nature07378. S2CID 4372536. Retrieved 2 February 2013.
- ^ Paul H, Muhr J (1986). «Review of experimental cross sections for K-shell ionization by light ions». Physics Reports. 135 (2): 47–97. Bibcode:1986PhR…135…47P. doi:10.1016/0370-1573(86)90149-3.
- ^ Köhn C, Ebert U (2014). «Angular distribution of Bremsstrahlung photons and of positrons for calculations of terrestrial gamma-ray flashes and positron beams». Atmospheric Research. 135–136: 432–465. arXiv:1202.4879. Bibcode:2014AtmRe.135..432K. doi:10.1016/j.atmosres.2013.03.012. S2CID 10679475.
- ^ Köhn C, Ebert U (2015). «Calculation of beams of positrons, neutrons, and protons associated with terrestrial gamma ray flashes». Journal of Geophysical Research: Atmospheres. 120 (4): 1620–1635. Bibcode:2015JGRD..120.1620K. doi:10.1002/2014JD022229.
- ^ Kochkin P, Köhn C, Ebert U, Van Deursen L (May 2016). «Analyzing x-ray emissions from meter-scale negative discharges in ambient air». Plasma Sources Science and Technology. 25 (4): 044002. Bibcode:2016PSST…25d4002K. doi:10.1088/0963-0252/25/4/044002. S2CID 43609721.
- ^ Cooray V, Arevalo L, Rahman M, Dwyer J, Rassoul H (2009). «On the possible origin of X-rays in long laboratory sparks». Journal of Atmospheric and Solar-Terrestrial Physics. 71 (17–18): 1890–1898. Bibcode:2009JASTP..71.1890C. doi:10.1016/j.jastp.2009.07.010.
- ^ Köhn C, Chanrion O, Neubert T (March 2017). «Electron acceleration during streamer collisions in air». Geophysical Research Letters. 44 (5): 2604–2613. Bibcode:2017GeoRL..44.2604K. doi:10.1002/2016GL072216. PMC 5405581. PMID 28503005.
- ^ Köhn C, Chanrion O, Babich LP, Neubert T (2018). «Streamer properties and associated x-rays in perturbed air». Plasma Sources Science and Technology. 27 (1): 015017. Bibcode:2018PSST…27a5017K. doi:10.1088/1361-6595/aaa5d8.
- ^ Köhn C, Chanrion O, Neubert T (May 2018). «High-Energy Emissions Induced by Air Density Fluctuations of Discharges». Geophysical Research Letters. 45 (10): 5194–5203. Bibcode:2018GeoRL..45.5194K. doi:10.1029/2018GL077788. PMC 6049893. PMID 30034044.
- ^ Förster A, Brandstetter S, Schulze-Briese C (June 2019). «Transforming X-ray detection with hybrid photon counting detectors». Philosophical Transactions. Series A, Mathematical, Physical, and Engineering Sciences. 377 (2147): 20180241. Bibcode:2019RSPTA.37780241F. doi:10.1098/rsta.2018.0241. PMC 6501887. PMID 31030653.
- ^ «Roentgen’s discovery of the x-ray». www.bl.uk. Retrieved 2019-05-09.
- ^ a b Roobottom CA, Mitchell G, Morgan-Hughes G (November 2010). «Radiation-reduction strategies in cardiac computed tomographic angiography». Clinical Radiology. 65 (11): 859–867. doi:10.1016/j.crad.2010.04.021. PMID 20933639.
Of the 5 billion imaging investigations performed worldwide…
- ^ a b «Medical Radiation Exposure Of The U.S. Population Greatly Increased Since The Early 1980s». ScienceDaily. Retrieved 2022-01-24.
- ^ Van Haver A, Kolk S, DeBoodt S, Valkering K, Verdonk P (2018). «Accuracy of total knee implant position assessment based on postoperative X-rays, registered to pre-operative CT-based 3D models». Orthopaedic Proceedings. 99-B (Supp 4).
- ^ Herman GT (2009). Fundamentals of Computerized Tomography: Image Reconstruction from Projections (2nd ed.). Springer. ISBN 978-1-85233-617-2.
- ^ Advances in kilovoltage x-ray beam dosimetry in Hill R, Healy B, Holloway L, Kuncic Z, Thwaites D, Baldock C (March 2014). «Advances in kilovoltage x-ray beam dosimetry». Physics in Medicine and Biology. 59 (6): R183–R231. Bibcode:2014PMB….59R.183H. doi:10.1088/0031-9155/59/6/r183. PMID 24584183. S2CID 18082594.
- ^ Thwaites DI, Tuohy JB (July 2006). «Back to the future: the history and development of the clinical linear accelerator». Physics in Medicine and Biology. 51 (13): R343–R362. Bibcode:2006PMB….51R.343T. doi:10.1088/0031-9155/51/13/R20. PMID 16790912. S2CID 7672187.
- ^ Hall EJ, Brenner DJ (May 2008). «Cancer risks from diagnostic radiology». The British Journal of Radiology. 81 (965): 362–378. doi:10.1259/bjr/01948454. PMID 18440940.
- ^ Brenner DJ (2010). «Should we be concerned about the rapid increase in CT usage?». Reviews on Environmental Health. 25 (1): 63–68. doi:10.1515/REVEH.2010.25.1.63. PMID 20429161. S2CID 17264651.
- ^ De Santis M, Cesari E, Nobili E, Straface G, Cavaliere AF, Caruso A (September 2007). «Radiation effects on development». Birth Defects Research. Part C, Embryo Today. 81 (3): 177–182. doi:10.1002/bdrc.20099. PMID 17963274.
- ^ «11th Report on Carcinogens». Ntp.niehs.nih.gov. Archived from the original on 2010-12-09. Retrieved 2010-11-08.
- ^ a b c Brenner DJ, Hall EJ (November 2007). «Computed tomography—an increasing source of radiation exposure». The New England Journal of Medicine. 357 (22): 2277–2284. doi:10.1056/NEJMra072149. PMID 18046031. S2CID 2760372.
- ^ Upton AC (July 2003). «The state of the art in the 1990’s: NCRP Report No. 136 on the scientific bases for linearity in the dose-response relationship for ionizing radiation». Health Physics. 85 (1): 15–22. doi:10.1097/00004032-200307000-00005. PMID 12852466. S2CID 13301920.
- ^ Calabrese EJ, Baldwin LA (February 2003). «Toxicology rethinks its central belief» (PDF). Nature. 421 (6924): 691–692. Bibcode:2003Natur.421..691C. doi:10.1038/421691a. PMID 12610596. S2CID 4419048. Archived from the original (PDF) on 2011-09-12.
- ^ Oakley PA, Ehsani NN, Harrison DE (2019-04-01). «The Scoliosis Quandary: Are Radiation Exposures From Repeated X-Rays Harmful?». Dose-Response. 17 (2): 1559325819852810. doi:10.1177/1559325819852810. PMC 6560808. PMID 31217755.
- ^ Berrington de González A, Darby S (January 2004). «Risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries». Lancet. 363 (9406): 345–351. doi:10.1016/S0140-6736(04)15433-0. PMID 15070562. S2CID 8516754.
- ^ a b Radiology (ACR), Radiological Society of North America (RSNA) and American College of. «Radiation Dose in X-Ray and CT Exams». Radiologyinfo.org. Retrieved 2022-01-24.
- ^ «National Cancer Institute: Surveillance Epidemiology and End Results (SEER) data». Seer.cancer.gov. 2010-06-30. Retrieved 2011-11-08.
- ^ Caon M, Bibbo G, Pattison J (2000). «Monte Carlo calculated effective dose to teenage girls from computed tomography examinations». Radiation Protection Dosimetry. 90 (4): 445–448. doi:10.1093/oxfordjournals.rpd.a033172.
- ^ Shrimpton, P.C; Miller, H.C; Lewis, M.A; Dunn, M. Doses from Computed Tomography (CT) examinations in the UK – 2003 Review Archived September 22, 2011, at the Wayback Machine
- ^ Gregory KJ, Bibbo G, Pattison JE (August 2008). «On the uncertainties in effective dose estimates of adult CT head scans». Medical Physics. 35 (8): 3501–3510. Bibcode:2008MedPh..35.3501G. doi:10.1118/1.2952359. PMID 18777910.
- ^ Giles D, Hewitt D, Stewart A, Webb J (September 1956). «Malignant disease in childhood and diagnostic irradiation in utero». Lancet. 271 (6940): 447. doi:10.1016/S0140-6736(56)91923-7. PMID 13358242.
- ^ «Pregnant Women and Radiation Exposure». eMedicine Live online medical consultation. Medscape. 28 December 2008. Archived from the original on January 23, 2009. Retrieved 2009-01-16.
- ^ a b c Ratnapalan S, Bentur Y, Koren G (December 2008). ««Doctor, will that x-ray harm my unborn child?»«. CMAJ. 179 (12): 1293–1296. doi:10.1503/cmaj.080247. PMC 2585137. PMID 19047611.
- ^ Donnelly LF (February 2005). «Reducing radiation dose associated with pediatric CT by decreasing unnecessary examinations». AJR. American Journal of Roentgenology. 184 (2): 655–657. doi:10.2214/ajr.184.2.01840655. PMID 15671393.
- ^ US National Research Council (2006). Health Risks from Low Levels of Ionizing Radiation, BEIR 7 phase 2. National Academies Press. pp. 5, fig.PS–2. ISBN 978-0-309-09156-5., data credited to NCRP (US National Committee on Radiation Protection) 1987
- ^ «ANS / Public Information / Resources / Radiation Dose Calculator». Archived from the original on 2012-05-16. Retrieved 2012-05-16.
- ^ «HOW DANGEROUS IS RADIATION?». www.phyast.pitt.edu. Retrieved 2022-01-24.
- ^ Muller, Richard. Physics for Future Presidents, Princeton University Press, 2010
- ^ X-Rays Archived 2007-03-15 at the Wayback Machine. Doctorspiller.com (2007-05-09). Retrieved on 2011-05-05.
- ^ X-Ray Safety Archived April 4, 2007, at the Wayback Machine. Dentalgentlecare.com (2008-02-06). Retrieved on 2011-05-05.
- ^ «Dental X-Rays». Idaho State University. Retrieved November 7, 2012.
- ^ D.O.E. – About Radiation Archived April 27, 2012, at the Wayback Machine
- ^ Chalkley M, Listl S (March 2018). «First do no harm — The impact of financial incentives on dental X-rays». Journal of Health Economics. 58 (March 2018): 1–9. doi:10.1016/j.jhealeco.2017.12.005. PMID 29408150.
- ^ «Using lasers instead of x-rays». Open University. 24 February 2011. Retrieved 28 July 2021.
- ^ Dent S (12 February 2015). «Scientists achieve X-ray vision with safe, visible light». Engadget. Retrieved 28 July 2021.
- ^ Kasai N, Kakudo, M (2005). X-ray diffraction by macromolecules. Tokyo: Kodansha. pp. 291–2. ISBN 978-3-540-25317-4.
- ^ Monico L, Van der Snickt G, Janssens K, De Nolf W, Miliani C, Verbeeck J, et al. (February 2011). «Degradation process of lead chromate in paintings by Vincent van Gogh studied by means of synchrotron X-ray spectromicroscopy and related methods. 1. Artificially aged model samples». Analytical Chemistry. 83 (4): 1214–1223. doi:10.1021/ac102424h. PMID 21314201. Monico L, Van der Snickt G, Janssens K, De Nolf W, Miliani C, Dik J, et al. (February 2011). «Degradation process of lead chromate in paintings by Vincent van Gogh studied by means of synchrotron X-ray spectromicroscopy and related methods. 2. Original paint layer samples». Analytical Chemistry. 83 (4): 1224–1231. doi:10.1021/ac1025122. PMID 21314202.
- ^ Ahi K, Anwar M (May 2016). «Advanced terahertz techniques for quality control and counterfeit detection». In Anwar MF, Crowe TW, Manzur T (eds.). Terahertz Physics, Devices, and Systems X: Advanced Applications in Industry and Defense. Vol. 9856. Society of Photographic Instrumentation Engineers. pp. 31–44.
- ^ Bickmore, Helen (2003). Milady’s Hair Removal Techniques: A Comprehensive Manual. ISBN 978-1401815554.
- ^ Frame P. «Wilhelm Röntgen and the Invisible Light». Tales from the Atomic Age. Oak Ridge Associated Universities. Retrieved 2021-10-11.
- ^ European Synchrotron Radiation Facility ID11
- ^ Als-Nielsen, Jens; Mcmorrow, Des (2001). Elements of Modern X-Ray Physics. John Wiley & Sons Ltd. pp. 40–41. ISBN 978-0-471-49858-2.
External links[edit]
- «On a New Kind of Rays». Nature. 53 (1369): 274–276. January 1896. Bibcode:1896Natur..53R.274.. doi:10.1038/053274b0.
- «Ion X-Ray tubes». The Cathode Ray Tube site.
- «Index of Early Bremsstrahlung Articles». Shade Tree Physics. 12 April 2010.
- Samuel JJ (20 October 2013). «La découverte des rayons X par Röntgen». Bibnum Education (in French). Röntgen’s discovery of X-rays (PDF; English translation)
- Oakley, P. A., Navid Ehsani, N., & Harrison, D. E. (2020). 5 Reasons Why Scoliosis X-Rays Are Not Harmful. Dose-Response. https://doi.org/10.1177/1559325820957797
Определение и разбор слова.
Данное слово является существительным, которое обычно употребляется в значении “метод неинвазивного лучевого исследования внутренних органов и скелета человека”.
Варианты написания.
При использовании этого слова в письме может возникнуть вопрос: «Какой вариант написания слова является правильным?»
— «рентген», где пишется непроизносимая согласная «т»
— «ренген», где непроизносимая согласная «т» не пишется
Как правильно пишется: «рентген» или «ренген»?
С точки зрения правил русской орфографии верным является следующее написание слова:
«РЕНТГЕН»
Какое правило применяется?
Данное слово является словарным, поэтому его правописание следует просто запомнить.
Пример использования слова в речи:
— Врач внимательно изучил мой рентген.
— Врач направил меня на рентген шейного отдела позвоночника.
— Последний раз рентген я делал два года назад.
Подводим итоги:
— Верное написание: «рентген»
— Неверное написание: «ренген»
Рентген:
- Рентген (Р) — внесистемная единица экспозиционной дозы радиоактивного облучения рентгеновским или гамма-излучением.
- Рентге́н — распространённый в русском языке вариант написания фамилии немецкого физика Вильгельма Конрада Рёнтгена, открывшего рентгеновское излучение.
- Рентген (в разговорной речи) — метод неинвазивного лучевого исследования внутренних органов — рентгенография и рентгеноскопия, а также аппарат для этого исследования.
- Рентген (шахматы) — тактический приём в шахматах.
- Рентген — большой ударный кратер в северном полушарии обратной стороны Луны.
- Рентген, Вильгельм Конрад (1845—1923) — немецкий физик.
См. также
- Рентгеновское излучение
- Рёнтген
Эта страница в последний раз была отредактирована 24 февраля 2023 в 12:22.
Как только страница обновилась в Википедии она обновляется в Вики 2.
Обычно почти сразу, изредка в течении часа.
Морфемный разбор слова:
Однокоренные слова к слову:
Рентген (единица измерения)
Рентге́н — внесистемная единица экспозиционной дозы радиоактивного облучения рентгеновским или гамма-излучением, определяемая по их ионизирующему действию на сухой атмосферный воздух. Международное обозначение — R, русское — P. В переводе на метрическую систему 1 Р приблизительно равен 0,0098 Зв
Содержание
Численное значение
1 Кл/кг = 3876 Р; 1 Р = 2,57976·10 −4 Кл/кг. [2]
Область применения
Принята в 1928 году. Несмотря на то, что, например, ГОСТ 8.417—81 прямо запретил использование большинства внесистемных единиц измерения, рентген продолжает достаточно широко использоваться в технике, отчасти потому, что многие [источник не указан 633 дня] имеющиеся измерительные приборы (дозиметры) отградуированы именно в рентгенах. Впрочем, широкого распространения единица Кл/кг не получила в связи с выходом из употребления самой физической величины экспозиционной дозы. Кл/кг используется главным образом для формального перевода из рентген в системные единицы (там, где исходная величина указана в единицах экспозиционной дозы). На практике сейчас чаще пользуются системными единицами поглощённой, эквивалентной и эффективной (а также групповой, коллективной, амбиентной и др.) дозы, то есть грэями и зивертами (а также кратными/дольными производными от них).
В условиях электронного равновесия (сумма энергий образующихся электронов, покидающих данный объем, равна сумме энергий электронов, поступающих в объем) экспозиционной дозе 1 Р соответствует поглощённая доза в воздухе, равная 0,88 рад (однако эта величина отличается от дозы, которую получил бы человек, если бы он находился в таком же поле излучения — как от поглощённой дозы в ткани, так и от амбиентного эквивалента дозы Н*(d)!).
Источник
Что такое рентгенография
Изобретенный более ста лет назад уникальный метод неинвазивного исследования внутренних органов – рентгенография – в настоящее время применяется для диагностики различных патологий в таких областях медицины, как остеология, неврология, пульмонология, оториноларингология, кардиология, гастроэнтерология, урология, гинекология, стоматология.
Хотя бы раз в жизни рентгеновский снимок приходится сделать каждому человеку. Что же при этом происходит и почему этот диагностический метод так популярен?
Что такое рентгенография?
Рентгенография – это исследование внутренней структуры тела путем просвечивания его рентгеновскими лучами и фиксирование результатов на специальную пленку. История рентгенологии началась в 1895 году. Именно тогда Вильгельмом Конрадом Рентгеном впервые было зарегистрировано затемнение фотопластинки под воздействием рентгеновского излучения. Он же установил, что рентгеновские лучи при прохождении различных тканей ослабляются по-разному, и за счет этого на фотопластинке можно получить различные изображения – например, костного скелета. Рентгенография стала первым в мире неинвазивным методом исследования внутренних органов и тканей.
Вплоть до настоящего времени рентгенография является основным методом диагностики при патологиях костно-суставной системы. Также важную роль этот метод играет при обследовании легких. Для оценки состояния внутреннего рельефа полых органов делается контрастная рентгенография. Принцип рентгенографии лег в основу более сложных современных исследований – например, компьютерной томографии.
Хотя рентгеновское излучение является ионизирующим и может оказать негативное влияние на организм, единственным серьезным противопоказанием для рентгенографии является беременность, и то – в качестве перестраховки. В случае контрастных исследований важно удостовериться, что у пациента нет индивидуальной непереносимости контрастирующих веществ. Современные диагностические аппараты продуцируют настолько незначительные разовые дозы рентгеновских лучей, что такое облучение укладывается в рамки естественного радиационного фона.
Достоинства и недостатки метода
Как и любой другой метод исследования, рентгенография имеет свои плюсы и минусы. Высокая разрешающая способность рентгеновских пленок позволяет получать снимки с достаточной степенью детализации, по которым может быть определена степень активности патологического процесса и реакция окружающих тканей. Рентгенограмма является диагностическим документом и, сравнивая ее с последующими снимками, можно судить о динамике патологического процесса. Недостаток классического метода – невозможность оценить состояние органов, находящихся в движении, и большие временные затраты на обработку пленки.
Виды исследования
Рентгенография легких представляет собой снимок грудной клетки в прямой и/или боковых проекциях, позволяющий оценить наличие и степень патологических изменений в легочной ткани.
Подготовка к процедуре
Если пациенту назначена рентгенография пояснично-крестцового отдела позвоночника или органов брюшной полости, рекомендуется за два дня до исследования придерживаться бесшлаковой диеты, а накануне провести очистительную клизму или принять препарат «Фортранс». Остальные виды рентгенографии не требуют специальной подготовки пациента.
Особенности проведения рентгенографии
Рентгенографию проводят с помощью различных рентгеновских приборов, которые могут быть как крупногабаритными, так и небольшими. Как правило, при проведении исследования пациент находится в одной комнате, а врач-рентгенолог в смежной смотровой, откуда подает команды – например, задержать дыхание.
Контрастную рентгенографию обычно проводят утром, натощак или после легкого завтрака. Бесконтрастное исследование может быть назначено на любое время. Продолжительность процедуры составляет несколько минут, кроме случаев, когда требуется сделать серию снимков с заданной периодичностью. Отдельно требуется время на проявку, сушку и описание снимков.
Рентгенография может проводиться в положении пациента стоя, сидя или лежа, в зависимости от назначенного исследования. В область облучения не должны попасть металлические украшения или застежки, которые будут видны на рентгеновском снимке и исказят результаты.
Анализ результатов
Четкость и точность полученного рентгеновского снимка зависят от напряжения и силы тока в рентгеновской трубке и времени ее работы. Эти параметры должны выставляться индивидуально в зависимости от исследования и массогабаритных характеристик пациента. К каждому рентгеновскому аппарату прилагается таблица средних значений для различных органов и тканей, однако врачу-рентгенологу приходится их корректировать для каждого конкретного случая. От того, насколько правильно он это сделает, будет зависеть качество исследования. Также очень важна неподвижность пациента во время процедуры.
Запись изображения проводится на рентгеночувствительную пленку либо на цифровой носитель с помощью компьютера. Регистрация рентгеновских данных в цифровом виде пока еще стоит дорого, поэтому традиционные рентгеновские пленки не теряют своей актуальности и применяются повсеместно.
При описании рентгеновского снимка следует учитывать, что изображение формируется расходящимися пучками лучей, поэтому кроме полученных размеров исследуемых объектов анализу подлежат затемнения и просветления.
Где сделать рентген в Махачкале?
В нашем центре имеется современный аппарат, пройти рентгенографию в нашем центре – легко! Звоните и записывайтесь!
Источник
Поиск ответа
Уважаемая грамота, подскажите, как правильно написать экспресс- рентген- диагностика. Три слова через дефис?
Ответ справочной службы русского языка
Вы написали верно, с двумя дефисами.
Здравствуйте! Подскажите, пожалуйста, какой из этих вариантов правильный: рентгеноборудование /рентген оборудование/ рентген- оборудование/рентгенооборудование?
Ответ справочной службы русского языка
Верно дефисное написание: рентген- оборудование.
Ответ справочной службы русского языка
Словарная фиксация: рентген- установка. См.: Русский орфографический словарь РАН / Под ред. В. В. Лопатина, О. Е. Ивановой. – 4-е изд., испр. и доп. – М., 2012.
Здравствуйте! Рентгенхирургия это моя специальность. Именно такое написание слова мне больше нравится. Несколько лет назад мне попалась статья специалиста по русскому языку в научном журнале по нашей специальности. Он указал, что такое написание вполне возможно, но не объяснил почему, хотя заметил, что объяснение у него есть. К сожалению не могу найти эту статью. Большая часть врачей пишет через соединительную гласную «рентгенохирургия». В таком виде это слово у меня вызывает отторжение. Яндекс выдает примерно в два раза больше ссылок на рентгенохирургию чем на рентгенхирургию. Есть еще совсем редкое употребление через дефис » рентген- хирургия». Какое написание Вы считаете правильным? Какие аргументы могу я привести коллегам для защиты своего любимого варианта?
Ответ справочной службы русского языка
Здравствуйте!
Как правильно:
рентген- кабинет, рентгенокабинет или рентгенкабинет?
И аналогично: рентген(о)(-)лаборант?
Спасибо!
Ответ справочной службы русского языка
Правильно: рентген- кабинет, рентген- лаборант.
Здравствуйте! Еще раз повторяю вопрос. Как правильно: рентгенкабинет, рентгенокабинет или рентген- кабинет? Спасибо!
Ответ справочной службы русского языка
Ответ справочной службы русского языка
Правильно: _рентгеноаппарат, шприцев_ и в профессиональной речи _шприцов_.
Источник
На каком основании после «рентген» ставят дефис? Например: «рентген-кабинет», «рентген-аппарат» и т. п
Размышляя над вопросом Рентген-эндоваскулярный или Рентгенэндоваскулярный?, я задумался: «А почему вообще ставится дефис в словах: „рентген-кабинет“, „рентген-аппарат“ и т. п.?»
Gramota.ru рекомендует такое написание в своих ответах:
Ответ справочной службы русского языка
Правильно: рентген-кабинет, рентген-лаборант.
Ответ справочной службы русского языка
Верно дефисное написание: рентген-оборудование.
Но такое написание не подпадает ни под одно правило русского языка. Это что, какая-то укоренившаяся ошибка?
«Рентген-кабинет» — это сложносокращённое слово от «рентгеновский кабинет», а «рентген-аппарат» — от «рентгеновский аппарат» и т. д.
По правилам русского языка сложносокращённые слова пишутся слитно, например: «стоматологический кабинет» — «стоматкабинет».
«Рентгеновский кабинет» должен писаться в сложносокращённом виде «рентгенкабинет», «рентгеновский аппарат» — «рентгенаппарат» и т. д. Если посчитать такие слова сложными, то: «рентгенокабинет», «рентгеноаппарат» и т. д.
Возможно, те, кто так пишут, руководствуются правилом:
сложные существительные, образованные без соединительной гласной, каждая часть которых может употребляться как самостоятельное слово;
Однако самостоятельного слова «рентген» в литературном русском языке нет, кроме фамилии изобретателя рентгеновских лучей Вильгельма Конрада Рёнтгена.
Разг. То же, что рентгеновские лучи (см. рентгеновский). Перед просмотром рентгеном сестра Ивановская сняла толстую пропитанную кровью повязку с головы лейтенанта. Емельянова, Хирург. || Просвечивание этими лучами. — Рентген показал изменение костной ткани в области шестого грудного позвонка. Коптяева, Иван Иванович.
Разг. Аппарат для просвечивания этими лучами.
Спец. Внесистемная единица измерения рентгеновского и гамма-излучений.
[Словарь русского языка Евгеньевой]
«Рентген» — это разговорное слово, т. е. просторечие, которым называют сами рентгеновские лучи или просвечивание ими.
Если кому-то не нравится приведённый словарь, вот ссылка на БТС, там точно так же слово «рентген» дано как разговорное.
Таким образом, нельзя писать «рентген-кабинет» через дефис, основываясь на том, что есть самостоятельное слово «рентген».
Почему же так пишут? Да ещё и внесли в орфографический словарь!
Источник
В чем разница между рентгенографией легких и флюорографией
Современные методы лучевой диагностики резко расширили границы визуализации внутренних структур тела. Сегодня в медицинской практике практически все анатомические зоны доступны для исследований. Как правило, лечащий врач определяет метод диагностики для постановки диагноза и при динамическом наблюдении пациента. Он также формирует план лечения и этапы сопровождения пациента на основании принципов надлежащей врачебной практики и доказательной медицины.

Однако не всегда вид медицинского исследования определяется только врачом, пациент сам вправе выбирать метод диагностики при профилактическом или диспансерном наблюдении. Примером самостоятельного принятия зачастую он основывает свои предпочтения исключительно на обилии «медицинской информации» в социальных ресурсах.
Сравним данные виды исследований
Рентгенография органов грудной клетки (рентгенография ОГК) – основной метод рентгенологического исследования, который проводится для диагностики патологии органов грудной клетки (легких, дыхательных путей, сердца, кровеносных сосудов, костей грудной клетки и позвоночника, пищевода). При данном исследовании изображение формируется в зависимости от поглощающей способности тканей, находящихся на пути прохождения рентгеновских лучей. Оно фиксируется на специальной рентгеновской пленке или на цифровом носителе информации.
Очевидным преимуществом метода является высокая разрешающая способность – рентгенографическое изображение определяет тени размером 1,5-2 мм. А в случае цифровых рентгенологических установок, еще и низкая лучевая нагрузка – эффективная эквивалентная доза (ЭЭД) облучения равна 0,1-0,2 мЗв. Метод цифрового рентгенологического исследования ОГК применяется как при массовых и скрининговых исследованиях, так и в качестве основного метода лучевой диагностики патологии органов грудной полости.
Флюорография – исключительно массовый (диспансерный) метод рентгенологического исследования заболеваний легких, в первую очередь рака и туберкулеза. При нем изображения теней фиксируется с рентгенографического экрана или оптического прибора на пленку маленького формата, которое в дальнейшем оценивается врачом рентгенологом с использованием средств увеличения изображения.
По сравнению с рентгенографией ОКГ разрешающая способность флюорографии позволяет определять тени размерами от 5 мм. Если выявляются негативные рентгенологические синдромы или подозрения на них, пациент направляется на дальнейшую диагностику, именно на выполнение рентгенографии ОГК. Пленочная флюорография получила широкое распространение лишь в массовых профилактических мероприятиях на территории советского и постсоветского пространства, прежде всего из экономической целесообразности, поскольку обладала низкой себестоимостью.
В корпусе клиники «Семейный доктор» на Бауманской рентген-диагностика выполняется с помощью полнофункционального рентген-аппарата последнего поколения ARCOMA Intuition (Швеция). Его использование позволяет добиться безошибочной диагностической точности получаемых изображений. Это первый в мире потолочный рентген-комплекс с полностью автоматическим позиционированием.
Источник
Теперь вы знаете какие однокоренные слова подходят к слову Как коротко пишется рентген, а так же какой у него корень, приставка, суффикс и окончание. Вы можете дополнить список однокоренных слов к слову «Как коротко пишется рентген», предложив свой вариант в комментариях ниже, а также выразить свое несогласие проведенным с морфемным разбором.
У этого термина существуют и другие значения, см. Рентген.
Рентге́н — внесистемная единица экспозиционной дозы радиоактивного облучения рентгеновским или гамма-излучением, определяемая по их ионизирующему действию на сухой атмосферный воздух. Международное обозначение — R, русское — P. В переводе на метрическую систему 1 Р приблизительно равен 0,0098 Зв
Численное значение
1 рентген — доза фотонного излучения, образующего ионы, несущие 1 ед. заряда СГСЭ ((1/3)·10−9 кулон) в 1 см³ воздуха при нормальном атмосферном давлении и 0 °C. В воздухе в 1см³ образуется 2,08·109 пар ионов[1].
Системная единица — кулон на килограмм (C/kg, Кл/кг).
- 1 Кл/кг = 3876 Р; 1 Р = 2,57976·10−4 Кл/кг.[2]
Область применения
|
|
В этом разделе не хватает ссылок на источники информации.
Информация должна быть проверяема, иначе она может быть поставлена под сомнение и удалена. |
Принята в 1928 году. Несмотря на то, что, например, ГОСТ 8.417—81 прямо запретил использование большинства внесистемных единиц измерения, рентген продолжает достаточно широко использоваться в технике, отчасти потому, что многие[источник не указан 633 дня] имеющиеся измерительные приборы (дозиметры) отградуированы именно в рентгенах. Впрочем, широкого распространения единица Кл/кг не получила в связи с выходом из употребления самой физической величины экспозиционной дозы. Кл/кг используется главным образом для формального перевода из рентген в системные единицы (там, где исходная величина указана в единицах экспозиционной дозы). На практике сейчас чаще пользуются системными единицами поглощённой, эквивалентной и эффективной (а также групповой, коллективной, амбиентной и др.) дозы, то есть грэями и зивертами (а также кратными/дольными производными от них).
В условиях электронного равновесия (сумма энергий образующихся электронов, покидающих данный объем, равна сумме энергий электронов, поступающих в объем) экспозиционной дозе 1 Р соответствует поглощённая доза в воздухе, равная 0,88 рад (однако эта величина отличается от дозы, которую получил бы человек, если бы он находился в таком же поле излучения — как от поглощённой дозы в ткани, так и от амбиентного эквивалента дозы Н*(d)!).
См. также
- Рад
- Грэй
- Зиверт
- Бэр — биологический эквивалент рентгена
- Фэр — физический эквивалент рентгена
Примечания
- ↑ Голубев Б. П. Дозиметрия и защита от ионизирующих излучений. 4-е изд (1986)
- ↑ Физическая энциклопедия. Рентген.
Ссылки
|
|
В этой статье не хватает ссылок на источники информации.
Информация должна быть проверяема, иначе она может быть поставлена под сомнение и удалена. |
Материал из Википедии — свободной энциклопедии
Перейти к навигации
Перейти к поиску
Рентген:
- Рентген (Р) — внесистемная единица экспозиционной дозы радиоактивного облучения рентгеновским или гамма-излучением.
- Рентге́н — распространённый в русском языке вариант написания фамилии немецкого физика Вильгельма Конрада Рёнтгена, открывшего рентгеновское излучение.
- Рентген (в разговорной речи) — метод неинвазивного лучевого исследования внутренних органов — рентгенография и рентгеноскопия, а также аппарат для этого исследования.
- Рентген (шахматы) — тактический приём в шахматах.
- Рентген — большой ударный кратер в северном полушарии обратной стороны Луны.
- Рентген, Вильгельм Конрад (1845—1923) — немецкий физик.
См. также[править | править код]
- Рентгеновское излучение
- Рёнтген:
- Рёнтген, Вильгельм Конрад (1845—1923) — немецкий физик.
- Рёнтген, Давид (1743—1807) — европейский мебельный мастер.
- Рёнтген, Энгельберт (1829—1897) — немецкий скрипач.
- Рёнтген, Юлиус (1855—1932) — нидерландский композитор, пианист, дирижёр, фольклорист и педагог немецкого происхождения.
- Рёнтген, Юлиус (младший) (1881—1951) — нидерландский скрипач немецкого происхождения.
-
- двойная фамилия
- Рёнтген-Майер, Аманда (1853—1894) — швейцарская скрипачка и композитор.
Источник — https://ru.wikipedia.org/w/index.php?title=Рентген&oldid=101376157
Категории:
- Страницы значений:Однофамильцы
- Страницы значений по алфавиту
Рентгеновские лучи относятся к особому виду электромагнитных колебаний, которые создаются в трубке рентгеновского аппарата, во время внезапной остановки электронов. Рентген — это знакомая многим процедура, но некоторые хотят знать о ней больше. Что такое рентген? Как делают рентген?
Свойства рентгена
В медицинской практике нашли применение такие свойства рентгена:
- Огромная проникающая способность. Рентгеновские лучи успешно проходят сквозь различные ткани человеческого организма.
- Рентген вызывает светоотражение отдельных химических элементов. Это свойство лежит в основе рентгеноскопии.
- Фотохимическое воздействие ионизирующих лучей позволяет создавать информативные, с диагностической точки зрения, снимки.
- Рентгеновское излучение обладает ионизирующим эффектом.
Во время рентгеновского сканирования различные органы, ткани и структуры выступают целевыми объектами для рентгеновских лучей. За время незначительной радиоактивной нагрузки может нарушаться обмен веществ, а при длительном воздействии радиации может возникнуть острая или хроническая лучевая болезнь.
Рентген-аппарат
Рентгеновские аппараты – это устройства, которые применяются не только в диагностических и лечебных целях в медицине, но и в различных областях промышленности (дефектоскопы), а также в других сферах жизни человека.
Устройство рентгеновского аппарата:
- трубки-излучатели (лампа) — одна или несколько штук;
- питающее устройство, которое питает аппарат электроэнергией, и регулирует параметры радиации;
- штативы, которые облегчают управление устройством;
- преобразователи рентгеновского излучения в видимое изображение.
Рентгеновские аппараты делятся на несколько групп в зависимости от того, как они устроены и где используются:
- стационарные – ими, как правило, оборудованы кабинеты в рентгенологических отделениях и поликлиниках;
- мобильные – предназначены для использования в отделениях хирургии и травматологии, в палатах интенсивной терапии и амбулаторно;
- переносные, дентальные (используются стоматологами).
При прохождении сквозь человеческое тело рентгеновские лучи проецируются на пленке. Однако угол отражения волн может быть различным и это сказывается на качестве изображения. На снимках лучше всего видны кости – ярко-белого цвета. Это связано с тем, что кальций больше всего поглощает рентгеновские лучи.
Виды диагностики
В медицинской практике рентгеновские лучи нашли применение в таких диагностических методах:
- Рентгеноскопия – это метод исследования, в ходе которого в прошлом обследуемые органы проецировалось на экран, покрытый флуоресцентным соединением. В процессе можно было исследовать орган под разными углами в динамике. А благодаря современной цифровой обработке сразу же получают готовое видеоизображение на мониторе или выводят его на бумагу.
- Рентгенография – это основной вид исследования. На руки пациенту выдается пленка с фиксированным снимком обследуемого органа или части тела.
- Рентгенография и рентгеноскопия с контрастом. Такой вид диагностики незаменим при исследовании полых органов и мягких тканей.
- Флюорография – это обследование с малоформатными рентгеновскими снимками, которые позволяют использовать его массово во время профилактических осмотров легких.
- Компьютерная томография (КТ) – диагностический метод, который позволяет подробно изучить человеческий организм за счет сочетания рентгена и цифровой обработки. Происходит компьютерная реконструкция послойных рентгенологических снимков. Из всех методов лучевой диагностики – этот наиболее информативный.
Рентгеновские лучи применяют не только для диагностики, но и для терапии. При лечении онкологических больных широко используется лучевая терапия.
В случае оказания неотложной помощи больному изначально делается обзорная рентгенография
Выделяют такие виды рентгенологического исследования:
- позвоночника и периферических отделов скелета;
- грудной клетки;
- брюшной полости;
- развёрнутое изображение всех зубов с челюстями, прилежащими отделами лицевого скелета;
- проверка проходимости маточных труб с помощью рентгена;
- рентгенологическое исследование молочной железы с невысокой долей излучения;
- рентгеноконтрастное исследование желудка и двенадцатиперстной кишки;
- диагностика желчного пузыря и протоков с применением контраста;
- исследование толстой кишки с ретроградным введением в нее рентгеноконтрастного препарата.
Рентген брюшной полости разделяют на обзорную рентгенографию и процедуру, выполняемую с применением контраста. Для определения патологий в легком широкое применение нашла рентгеноскопия. Рентгенографическое исследование позвоночника, суставов и других частей скелета – является очень популярным методом диагностики.
Неврологи, травматологи и ортопеды не могут поставить своим пациентам точный диагноз, не воспользовавшись таким видом обследования. Показывает рентген грыжу позвоночника, сколиоз, различные микротравмы, нарушения костно-связочного аппарата (патологии здоровой стопы), переломы (лучезапястного сустава) и многое другое.
Подготовка
Большая часть диагностических манипуляций, связанных с использованием рентгеновских лучей, не требует специальной подготовки, но есть и исключения. Если запланировано обследование желудка, кишечника или пояснично-крестцового отдела позвоночника, то за 2–3 дня до рентгенографии требуется придерживаться специальной диеты, которая снижает метеоризм и процессы брожения.
При обследовании ЖКТ требуется накануне диагностики и непосредственно в день обследования сделать очистительные клизмы классическим способом с помощью кружки Эсмарха или очистить кишечник с помощью аптечных слабительных (пероральные препараты или микроклизмы).
При обследовании органов брюшной полости минимум за 3 часа до процедуры нельзя кушать, пить, курить. Прежде чем отправляться на маммографию необходимо посетить гинеколога. Проводить рентгенологическое исследование груди следует в начале менструального цикла после окончания месячных. Если у женщины, которая планирует обследование груди, стоят импланты, то об это необходимо обязательно сообщить рентгенологу.
Проведение
Зайдя в рентген-кабинет он должен снять с себя элементы одежды или украшения, которые содержат металл, а также оставить вне кабинета мобильный телефон. Как правило, пациента просят раздеться до пояса, если обследуется грудная клетка или брюшина. Если же необходимо выполнить рентген конечностей, то пациент может оставаться в одежде. Все части тела, которые не подлежат диагностике, должны быть прикрыты защитным свинцовым фартуком.
Снимки могут выполняться в различных положениях. Но чаще всего пациент стоит или лежит. Если нужна серия снимков под разными углами, то рентгенолог дает пациенту команды о смене положения тела. Если выполняется рентген желудка, то больному понадобится занять положение Тренделенбурга.
Это особенная поза, при которой органы таза находятся немного выше головы. В результате манипуляций получают негативы, на которых видно светлые участки более плотных структур и темные, указывающие на наличие мягких тканей. Расшифровка и анализ каждой области тела выполняется по определенным правилам.
Детям довольно часто делается рентген для выявления дисплазии тазобедренных суставов
Частота проведения
Максимально допустимая эффективная доза радиации – 15 мЗв в год. Как правило, такую порцию облучения получают только люди, которые нуждаются в регулярном рентгенологическом контроле (после тяжёлых травм). Если же в течение года пациент делает только флюорографию, маммографию и рентген у стоматолога, то он может быть совершенно спокойным, поскольку его лучевая нагрузка не превысит и 1,5 мЗв.
Острая лучевая болезнь может возникнуть только в том случае, если человек однократно получит облучение в дозе – 1000 мЗв. Но если это не ликвидатор на атомной электростанции, то чтобы получить такую лучевую нагрузку, пациент в один день должен сделать 25 тысяч флюорографий и тысячу рентгеновских снимков позвоночника. А это нонсенс.
Те же дозы облучения, которые человек получает при стандартных обследования, даже при условии их повышенного количества не способны оказать заметного отрицательного воздействия на организм. Поэтому рентген можно делать настолько часто, насколько того требуют медицинские показания. Однако этот принцип не распространяется на беременных женщин.
Им рентген противопоказан на любом сроке, особенно в первом триместре, когда происходит закладка всех органов и систем у плода. Если же обстоятельства вынуждают сделать женщине рентген во время вынашивания ребенка (серьезные травмы во время ДТП), то стараются использовать максимальные меры защиты для живота и органов малого таза. Во время кормления грудью женщинам разрешается делать как рентген, так и флюорографию.
При этом, по мнению многих специалистов, ей даже не требуется сцеживать молоко. Флюорографию маленьким детям не делают. Эта процедура допустима с 15-летнего возраста. Что касается рентген-диагностики в педиатрии, то к ней прибегают, но учитывают, что дети обладают повышенной радиочувствительностью к ионизирующему излучению (в среднем в 2–3 раза выше чем взрослые), что создает у них высокий риск возникновения как соматических, так и генетических эффектов облучения.
Противопоказания
Рентгеноскопия и рентгенография органов и структур человеческого тела имеет не только множество показаний, но и ряд противопоказаний:
- туберкулез в активной форме;
- эндокринные патологии щитовидной железы;
- общее тяжелое состояние пациента;
- вынашивание ребенка на любом сроке;
- для рентгенографии с применением контраста – период лактации;
- серьезные нарушения в работе сердца и почек;
- внутренние кровотечения;
- индивидуальная непереносимость контрастных препаратов.
Сделать рентген в наше время можно во многих медцентрах. Если рентгенографической или рентгеноскопическое исследование делается на цифровых комплексах, то пациент может рассчитывать на меньшую дозу облучения. Но даже цифровой рентген может считаться безопасным, только в случае не превышения допустимой частоты выполнения процедуры.
Слитно или раздельно? Орфографический словарь-справочник. — М.: Русский язык . Б. З. Букчина, Л. П. Какалуцкая . 1998 .
Смотреть что такое «рентгенолаборант» в других словарях:
рентгенолаборант — сущ., кол во синонимов: 1 • лаборант (1) Словарь синонимов ASIS. В.Н. Тришин. 2013 … Словарь синонимов
Сре́дний медици́нский персона́л — лица, получившие специальное образование и соответствующую квалификацию в средних медицинских учебных заведениях и допущенные в установленном порядке к медицинской деятельности. В соответствии с уровнем и профилем образования С. м. п. оказывает… … Медицинская энциклопедия
Радиоло́гия интервенцио́нная — раздел медицинской радиологии, разрабатывающий научные основы и клиническое применение лечебных и диагностических манипуляций, осуществляемых под контролем лучевого исследования. Формирование Р. и. стало возможным с внедрением в медицину… … Медицинская энциклопедия
Метросальпингография — контрастное рентгенологическое исследование полости матки и проходимости фаллопиевых труб. Исследование проводится в рентгеновском кабинете при тщательном соблюдении правил асептики. Контрастное вещество (йодолипол) вводит с помощью специального… … Википедия
лаборант — сущ., кол во синонимов: 1 • рентгенолаборант (1) Словарь синонимов ASIS. В.Н. Тришин. 2013 … Словарь синонимов
Список награждённых медалью «За спасение погибавших», 2008 год — Приложение к статье Медаль «За спасение погибавших» Содержание 1 Респуб … Википедия
Орфографический словарь
рентг е н 1 , -а (рентгеноскопия, разг.)
рентг е н-аппар а т, -а и рентгеноаппар а т, -а
рентг е н-диагн о стика, -и и рентгенодиагн о стика, -и
рентг е н-излуч е ние, -я
рентг е н-кабин е т, -а
рентг е н-лабор а нт, -а
рентгеннегат и вный
рентг е новский
рентг е новы луч и , рентг е новых луч е й (от Рентг е н)
рентгеногр а мма, -ы
рентгенограф и ческий
рентгеногр а фия, -и
рентгенодефектоскоп и я, -и
Большой толковый словарь
РЕНТГ Е Н, -а; м. 1. Разг. =Рентгеновские лучи. Лечение рентгеном. Просвечивать рентгеном. // Просвечивание этими лучами. Назначить больного на р. Р. показал изменение костной ткани. 2. Разг. Аппарат для просвечивания этими лучами. Включить р. Поломка рентгена. 3. Спец. Внесистемная единица измерения рентгеновского или гамма-излучений. Уровень радиации составил тридцать рентгенов в час. ●По имени немецкого физика В.К. Рентгена (1845 — 1923).
РЕНТГ Е НОВ, -а, -о. ◊ Рентг е новы лучи. =Рентгеновские лучи.
РЕНТГ Е НОВСКИЙ, -ая, -ое. Рентг е новские лучи; рентг е новское излучение. Невидимые лучи, являющиеся короткими электромагнитными волнами, способными проникать через непрозрачные предметы. е новский, -ая, -ое. Сделанный при помощи таких лучей. Р. снимок. // Использующий в своей работе такие лучи. Р. микроскоп. // Предназначенный для размещения рентгена (2 зн.). Р. кабинет.
РЕНТГЕНОГР А ММА, -ы; ж. [от слова рентген и греч. grámma — запись, письменный знак] Изображение на фотопластинке или плёнке, полученное с помощью рентгеновских лучей. Р. показала затемнение в лёгких.
РЕНТГЕНОГР А ФИЯ, -и; ж. [от сл. рентген и греч. gráphō — пишу] Исследование внутреннего строения непрозрачных тел при помощи просвечивания их рентгеновскими лучами и фиксирования прошедших лучей на фотоплёнке. и ческий, -ая, -ое. Р-ое исследование. Р. центр.
РЕНТГЕНОДИАГН О СТИКА, -и; ж. Распознавание заболеваний тканей и органов с помощью рентгеновских лучей.
РЕНТГЕН О ЛОГ, -а; м. Врач — специалист по рентенологии и рентгенотерапии.
РЕНТГЕНОЛ О ГИЯ, -и; ж. [от сл. рентген и греч. lógos — учение] Раздел медицины, изучающий применение с диагностическими и лечебными целями рентгеновских лучей. и ческий, -ая, -ое. Р-ое исследование. Р. кабинет.
РЕНТГЕНОСКОП И Я, -и; ж. [от сл. рентген и греч. skopéō — смотрю] Просвечивание рентгеновскими лучами тел и рассматривание на особом экране их теневого изображения для исследования их внутреннего строения. Р. желудка. Сделать рентгеноскопию. и ческий, -ая, -ое. Р. метод. Р. аппарат.
РЕНТГЕНОТЕРАП И Я [тэ] и [те], -и; ж. [от сл. рентген и греч. therapéia — лечение] Использование рентгеновских лучей для лечения опухолевых и других заболеваний.
РЕНТГЕНОТ Е ХНИК, -а; м. Специалист по обслуживанию рентгеновского аппарата, рентгенотехники. и ческий (см.).
РЕНТГЕНОТ Е ХНИКА, -и; ж. Совокупность методов и технических средств для использования рентгеновского излучения в медицине, науке и технике.
РЕНТГЕНОТЕХН И ЧЕСКИЙ, -ая, -ое. к Рентгенот е хник и Рентгенот е хника. Р-ая лаборатория.
Управление в русском языке
Русское словесное ударение
рентг е н, -а; р. мн. -ов, счётн.ф. рентг е н [нг] (единица экспозиционной дозы рентгеновскогои гамма-излучений)
рентг е н, -а [нг] ( то же, что рентгеноскоп и я)
рентгениз и рованный, -ан, -ана, -ано,-аны [нг]
рентгениз и ровать, -з и рую, -з и руешь[нг]
рентг е ноаппар а т [нг]
рентг е новский [нг]
рентг е ногр а мма [нг]
рентгеногр а фия, -и [нг]
рентг е нодефектоскоп и я, -скоп и и [нг]
рентг е нодиагн о стика [нг]
рентг е ноким о граф [нг]
рентг е нокимогр а фия, -и [нг]
рентген о лог [нг]
рентгенол о гия, -и [нг]
рентген о метр [нг]
Словарь имён собственных
РЕНТГ Е Н (Рёнтген) Вильг е льм К о нрад, Рентг е на (Рёнтгена) Вильг е льма К о нрада
| Blurb |
|---|
| перед тем как задать вопрос, прочтите, пожалуйста, FAQ. уважайте чужое время. |
| FAQ |
| поиск |
| книга жалоб |
| словари на Грамоте.ру |
| энциклопедии и словари в интернете |
| словари русского языка для Lingvo |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| 8 | 9 | 10 | 11 | 12 | 13 | 14 |
| 15 | 16 | 17 | 18 | 19 | 20 | 21 |
| 22 | 23 | 24 | 25 | 26 | 27 | 28 |
| 29 | 30 | 31 |
| Свежие записи |
| Архив |
| Друзья |
| Личная информация |
| Поделиться |
| Пожаловаться |
| [#] (без темы) |
| [#] (без темы) |
| [#] (без темы) |
| [#] (без темы) |
Здравствуйте, уважаемые сообщники!
Засомневалась в написании одного слова, решила глянуть в нормативную базу — удивлению не было предела: сколько документов столько и мнений..
А Вы к чему более склоняетесь:
(все эти варианты звучат в различных и многих документах, причем неоднократно).
| From: |  oldasapujo oldasapujo |
|---|---|
| Date: | Октябрь, 12, 2007 10:35 (UTC) |
Adblock detector
Для диагностики различных заболеваний легких, костей и других органов и тканей человеческого организма в медицине на протяжении 120 лет используется рентгенография (или рентген) – это простая и безошибочная методика, позволившая спасти огромное количество жизней благодаря точности постановки диагноза и безопасности проведения процедуры.
Х-лучи, открытые немецким физиком Вильгельмом Рентгеном, почти беспрепятственно проходят через мягкие ткани. Костные структуры организма их не пропускают, в результате чего на рентгеновских снимках образуются тени разной интенсивности, точно отображающие состояние костей и внутренних органов.
Рентгенография – это одна из самых исследованных и проверенных в клинической практике техник диагностики, влияние которой на организм человека прекрасно изучено за более чем вековое применение в медицине. В России (в Петербурге и Киеве) благодаря этой методике уже в 1896 году, через год после открытия Х-лучей, были успешно проведены операции с использованием рентгеновских снимков на фотопластинах.
Что такое рентген
Несмотря на то, что современное рентгеновское оборудование постоянно совершенствуется и представляет собой высокоточные медицинские приборы, позволяющие проводить детальную диагностику, принцип получения снимка остался неизменным. Ткани человеческого организма, обладающие разной плотностью, пропускают невидимые Х-лучи с различной степенью интенсивности: мягкие здоровые структуры их практически не задерживают, а кости – поглощают. Итоговые снимки выглядят, как совокупность теневых изображений. Рентгеновский снимок является негативом, на котором белым цветом обозначены костные структуры, серым – мягкие, а черным – воздушные прослойки. Наличие патологических изменений во внутренних органах, например, в легких, отображается в виде более светлого места на легочной плевре или в сегментах самого легкого. Описание сделанной рентгенограммы является основанием, по которому врачи могут судить о состоянии тех или иных объектов исследования.
Если в XX веке аппаратура позволяла проводить, в основном, только исследование грудной клетки и конечностей, то современная рентгеноскопия применяется для высокоточной диагностики различных органов с помощью широкого модельного ряда рентгеновского оборудования.
Виды и проекции рентгенографии
Для проведения профилактических исследований и глубокой диагностики в медицине используются различные виды рентгенографии. Рентгеновские методики классифицируются:
- по форме:
- обзорная, позволяющая целиком охватывать различные области тела;
- прицельная, которую обычно проводят при глубокой диагностике определенного участка того или иного органа при помощи специальной насадки на рентгеновском аппарате;
- послойная, при проведении которой выполняются параллельные срезы исследуемой зоны.
- по типу используемого оборудования:
- традиционная пленочная;
- цифровая, предоставляющая возможность записывать полученное изображение на съемные носители;
- трехмерная. Сюда относятся компьютерная, мультиспиральная и другие виды томографии;
- флюорографическая, позволяющая проводить безопасное профилактическое обследование легких;
- специальные:
- маммографическая, для обследования молочной железы у женщин;
- гистеросальпингографическая, применяемая для обследования матки и маточных труб;
- денситометрическая, для диагностики остеопороза и другие.
Перечисление разнообразных методик показывает, какой востребованной и незаменимой в диагностике бывает рентгенология. Современные медики могут использовать различные формы исследований для выявления патологий в большинстве органов и жизненно важных систем человеческого тела.
Для чего делают рентген
Х-лучи в современной медицине применяются для профилактических осмотров и направленной диагностики. Без такого обследования не обойтись при:
- переломах костей;
- повреждении внутренних органов в результате внешнего травмирования;
- диагностике рака молочной железы и ряда других онкологических заболеваний;
- исследовании легких и других органов грудной клетки;
- лечении и протезировании зубов;
- глубоком изучении структур головного мозга;
- сканировании участков сосудов с подозрением на аневризму и так далее.
Методику проведения рентгенологического исследования выбирает врач в зависимости от наличия к ней показаний и противопоказаний у пациента. По сравнению с некоторыми современными методиками получения объемных изображений традиционный рентген является наиболее безопасным. Но и он не показан определенным категориям пациентов.
Противопоказания
Несмотря на безопасность диагностики, пациенты испытывают на себе действие ионизирующего излучения, которое отрицательно сказывается на костном мозге, эритроцитах, эпителии, репродуктивных органах и сетчатке глаза. Абсолютными противопоказаниями для проведения рентгена являются:
- беременность;
- возраст ребенка до 14 лет;
- тяжелое состояние больного;
- активная форма туберкулеза;
- пневмоторакс или кровотечение;
- болезни щитовидной железы.
Детям и беременным женщинам такое обследование назначается только в крайних случаях, когда угроза для жизни – больше, чем потенциальный вред от процедуры. По возможности стараются прибегнуть к альтернативным методикам. Так, если врачу нужно диагностировать опухоль у беременной, то вместо рентгена используется УЗИ.
Что нужно для рентгена в качестве подготовки
Для обследования состояния позвоночника, желудка или челюстных костей специальная подготовка не нужна. Пациенту необходимо снять с себя одежду и металлические предметы перед прохождением такого обследования. Отсутствие посторонних предметов на теле обеспечивает точность рентгеновского снимка.
Подготовка требуется только при использовании контрастного вещества, которое вводится для проведения рентгена тех или иных органов с целью повышения визуализации результатов. Инъекцию контрастирующего препарата делают за некоторое время до выполнения процедуры или непосредственно в процессе.
Как делают рентген
Все рентгеновские снимки делаются в специально оборудованных кабинетах, где имеются защитные экраны, предотвращающие попадание излучения на непросвечиваемые органы тела. Исследование не занимает много времени. В зависимости от того, по какой методике делается процедура, рентгенография выполняется в разных положениях. Пациент может стоять, лежать или сидеть.
Можно ли пройти на дому
Надлежащие условия съемки рентгеновским аппаратом той или иной модификации создаются в специально оборудованных кабинетах, где имеется защита от ионизирующих лучей. Такая аппаратура обладает большими габаритами и используется только в стационарных условиях, что позволяет добиваться максимальной безопасности процедуры.
Для проведения профилактических обследований большого количества людей на территориях, отдаленных от больших клиник, могут использоваться мобильные флюорографические кабинеты, которые полностью повторяют обстановку стационарных медицинских помещений.
Сколько раз можно делать рентген
Просвечивание тканей и органов проводится столько раз, сколько допускает та или иная методика диагностики. Наиболее безопасными считаются флюорография и рентген. Врач может направить пациента несколько раз на такое обследование в зависимости от полученных ранее результатов и поставленных целей. Объемные снимки делают по показаниям.
При назначении рентгенографии важно не превышать максимально разрешенную суммарную дозу радиации за год, равную 150 мЗв. Для информации: облучение при выполнении рентген-снимка грудной клетки в одной проекции составляет 0,15-0,4 мЗв.
Где можно сделать рентгеновский снимок, и его средняя стоимость
Рентгенограмму можно сделать практически в любом медицинском учреждении: в государственных поликлиниках, стационарах, частных центрах. Стоимость такого обследования зависит от исследуемой зоны и количества выполненных снимков. В рамках обязательного медицинского страхования или по выделенным квотам в государственных больницах просвечивание органов по направлению врача можно сделать бесплатно. В частных медицинских учреждениях такую услугу нужно будет оплатить. Цена начинается от 1500 рублей и в разных частных медцентрах может варьироваться.
Что показывает рентген
Что показывает выполненная рентгенография? На сделанном снимке или на экране монитора видно состояние определенного органа. Разнообразие темных и светлых оттенков на полученном негативе позволяет врачам судить о наличии или отсутствии тех или иных патологических изменений в определенном отделе исследуемого органа.
Расшифровка результатов
Читать рентгеновские снимки может только квалифицированный врач, имеющий длительную клиническую практику и разбирающийся в особенностях различных патологических изменений в тех или иных органах тела. На основе увиденного на снимке доктор делает описание полученной рентгенограммы в карте больного. При отсутствии нетипичных светлых пятен или затемнений на мягких тканях, трещин и переломов на костях медик фиксирует здоровое состояние того или иного органа. Точно расшифровать рентгеновский снимок может только опытный врач, прекрасно знающий рентгеноанатомию человека и симптомы заболевания того органа, снимок которого делается.
На что указывают воспалительные очаги на снимке
При просвечивании мягких тканей, суставов или костей при наличии патологических изменений в них появляются характерные для того или иного заболевания симптомы. Пораженный воспалением участок иначе поглощает рентгеновское излучение, чем здоровые ткани. Как правило, такая зона содержит выраженные очаги затемнений. Опытный доктор сразу определяет тип заболевания по полученному изображению на снимке.
Как выглядят заболевания на рентгеновском снимке
При переносе изображения на пленку места с патологическими изменениями выделяются на фоне здоровой ткани. При просвечивании поврежденных костей отчетливо видны места деформаций и смещений, что позволяет травматологу поставить точный прогноз и назначить правильное лечение. Если выявлены тени на легких, это может свидетельствовать о пневмонии, туберкулезе или раке. Квалифицированный специалист должен дифференцировать выявленные отклонения. А вот области просветления в этом органе зачастую свидетельствуют о плеврите. Специфические симптомы характерны для каждого вида патологии. Чтобы поставить правильный диагноз, необходимо в совершенстве владеть рентгеноанатомией человеческого тела.
Преимущества методики, и в чем негативное влияние рентгена на организм
Полученные в результате просвечивания Х-лучами рентгеновские снимки дают точное понимание состояния исследуемого органа и позволяют врачам поставить точный диагноз. Минимальная продолжительность такого обследования и современное оборудование существенно снижают возможность получения опасной для здоровья человека дозы ионизирующего облучения. Пары минут достаточно для детальной визуализации органа. За это время, при отсутствии противопоказаний у пациента, невозможно нанести непоправимый вред организму.
Как минимизировать последствия облучения
Все формы диагностики заболеваний с применением рентгеновских лучей проводятся только по медицинским показаниям. Наиболее безопасной считается флюорография, которую рекомендуется проходить ежегодно с целью раннего выявления и профилактики туберкулеза и рака легких. Все остальные процедуры назначаются с учетом интенсивности рентген-излучения, при этом информация о полученной дозе заносится в карту больного. Специалист всегда учитывает данный показатель при подборе диагностических методик, что позволяет не превышать норму.
Чтобы снизить последствия облучения, рекомендуется есть пищу, содержащую селен, калий, пектин и клетчатку, метионин, молоко и молочные продукты, мед.
Можно ли делать рентген детям
Согласно с международными и отечественными нормативами, любые исследования, основанные на воздействии ионизирующего излучения, разрешается проводить лицам, достигшим 14 лет. В качестве исключения врач может назначить ребенку рентгенографию только при подозрении у него на опасные болезни легких с согласия родителей. Такое обследование необходимо в острых ситуациях, требующих проведения быстрой и точной диагностики. Перед этим специалист всегда соотносит риски от процедуры и угрозу жизни ребенка в случае ее непроведения.
Возможен ли рентген при беременности
Такое обследование обычно не назначают в период вынашивания плода, особенно в первом триместре. Если оно необходимо настолько, что отсутствие своевременной диагностики угрожает здоровью и жизни будущей мамы, то в ходе его используется свинцовый фартук для защиты внутренних органов от Х-лучей. На фоне других аналогичных методов рентген – самый безопасный, но и его врачи предпочитают в большинстве случаев не проводить во время беременности, оберегая плод от пагубных ионизирующих воздействий.
Альтернатива рентгену
120-летняя практика использования рентгена и аналогичных методик (флюорографии, компьютерной, мультиспиральной, позитронно-эмиссионной томографии и прочих) показала, что на сегодняшний день не существует более точного способа диагностики ряда патологий. С помощью рентген-исследования можно быстро определить заболевания легких, травмы костей, выявить дивертикулы у возрастных пациентов, сделать качественную ретроградную уретрографию, своевременно обнаружить онкологию на начальной стадии развития и многое другое.
Альтернатива такой диагностике в виде УЗИ может назначаться только беременным женщинам или пациентам с противопоказаниями к проведению рентгена.
Ответ:
Правильное написание слова — рентгеновский
Ударение и произношение — рентг`еновский
Значение слова -относящийся к применению таких лучей
Пример:
Р. снимок. Р. кабинет.
Выберите, на какой слог падает ударение в слове — СОЗВОНИМСЯ?
или
Слово состоит из букв:
Р,
Е,
Н,
Т,
Г,
Е,
Н,
О,
В,
С,
К,
И,
Й,
Похожие слова:
рентабельный
рентген
рентгенизация
рентгенизированный
рентгенметр
рентгенограмма
рентгенографический
рентгенография
рентгенодефектоскопия
рентгенодиагностика
Рифма к слову рентгеновский
семеновский, измайловский, понятовский, козловский, кутузовский, августовский, московский, платовский, раевский, пржебышевский, корчевский, георгиевский, киевский, поэтический, купеческий, панический, эгоистический, виртембергский, голландский, педантический, княжеский, героический, комический, фурштадский, ольденбургский, павлоградский, ребяческий, дипломатический, персидский, дружеский, сангвинический, политический, кавалергардский, логический, стратегический, адский, человеческий, шведский, электрический, иронический, энергический, физический, чарторижский, господский, нелогический, трагический, католический, исторический, фантастический, петербургский, робкий, ловкий, дикий, низкий, узкий, негромкий, одинокий, бойкий, звонкий, тонкий, крепкий, глубокий, великий, гладкий, жаркий, сладкий, жалкий, легкий, скользкий, пылкий, неловкий, невысокий, резкий, высокий, жестокий, близкий, некий, далекий, редкий, яркий, неробкий, широкий, громкий, дерзкий, краснорожий, удовольствий, георгий, препятствий, рыжий, похожий, строгий, орудий, приветствий, жребий, отлогий, бедствий, свежий, действий, происшествий, условий, сергий, пологий, божий, проезжий, религий, сословий, хорунжий, самолюбий, непохожий, дивизий, кривоногий, толсторожий, муругий, последствий, приезжий
Толкование слова. Правильное произношение слова. Значение слова.